Complexity of tumors revealed in 3D
Maps of tumor ‘neighborhoods’ open door to future treatment strategies
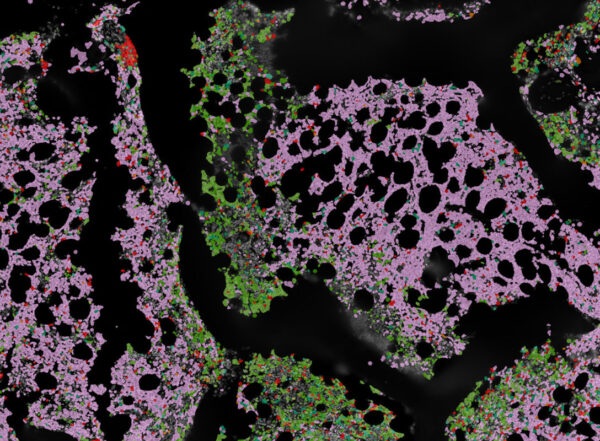
WashU MedicineResearchers at WashU Medicine have generated structural maps of tumors in three dimensions. These 3D cell atlases, published in Nature, reveal tumor organization at the single-cell level and provide opportunities for exploring new approaches to cancer therapy. Tumor images provided by Erik Storrs/Ding lab.
A new analysis led by researchers at Washington University School of Medicine in St. Louis has revealed detailed 3D maps of the internal structures of multiple tumor types. These cancer atlases reveal how different tumor cells — and the cells of a tumor’s surrounding environment — are organized, in 3D, and how that organization changes when a tumor spreads to other organs.
The detailed findings offer scientists valuable blueprints of tumors that could lead to new approaches to therapy and spark a new era in the field of cancer biology, according to the researchers.
The study is part of a group of 12 papers published Oct. 30 in the Nature suite of journals by members of the Human Tumor Atlas Network, a research consortium funded by the National Cancer Institute (NCI) of the National Institutes of Health (NIH). The 3D analysis — published in Nature — includes detailed data about breast, colorectal, pancreas, kidney, uterine and bile duct cancers.
The last decade of cancer research has been defined by tremendous advances in understanding the activities of cells in a tumor’s environment — both the cancer itself and its support cells, including on a single-cell level. The new study begins to reveal not just what each cell is up to, but also where each cell is located in the intact tumor and how each interacts with its neighboring cells, whether those cells are next door, down the street or in a completely different neighborhood.
This new information could help scientists understand how tumors spread or develop treatment resistance, to name a few intensive areas of ongoing study.
“These 3D maps of tumors are important because they finally let us see what, until now, we have only been able to infer about tumor structures and their complexity,” said co-senior author Li Ding, PhD, the David English Smith Professor of Medicine. “We understood that cancer cells, immune cells and structural cells were all present in the tumor, sometimes protecting the cancer from chemotherapy and immune system attack, but now we can actually see those battle lines. We now have the ability to see how regions of the tumor differ in 3D space and how the behavior changes in response to therapy or when the tumor spreads to other organs. These studies have opened a new era in cancer research with the potential to transform the way we understand and treat cancer in the future.”
The study is led by Ding, also a research member of Siteman Cancer Center, based at Barnes-Jewish Hospital and WashU Medicine; and her fellow co-senior authors Feng Chen, PhD, a professor of medicine; Ryan C. Fields, MD, the Kim and Tim Eberlein Distinguished Professor; William E. Gillanders, MD, a professor of surgery, all of WashU Medicine; and Benjamin J. Raphael, PhD, of Princeton University.
3D organization of tumor neighborhoods
In general, the researchers found that tumors had higher metabolic activity — that is, they burned more fuel — in their cores and more immune system activity on their edges. They also found that a tumor can contain multiple neighborhoods with different genetic mutations driving the tumor’s growth. These neighborhoods are being appreciated for how they lead to treatment response and resistance in various cancer types. This suggests different targeted treatments may be needed to address key mutations in different neighborhoods.
“This understanding of 3D cancer metabolism will affect how our current treatments work, and sometimes don’t work, and will lead to development of novel treatments in cancer,” said Fields, who treats patients at Siteman. “It really is transformative.”
In addition, some tumor neighborhoods can have high immune cell activity — known as hot regions. The same tumor also can have so-called cold regions that do not have much, if any, immune activity. Hot regions typically respond well to immunotherapies, but cold regions do not, possibly helping to explain why some tumors appear responsive to immunotherapies at first and then develop resistance. If various mutation profiles as well as cold and hot neighborhoods can be identified, it presents the possibility of designing treatment strategies that could be effective against all neighborhoods within the same tumor.
The researchers — including co-first authors, Chia-Kuei (Simon) Mo and Jingxian (Clara) Liu, both graduate students in Ding’s lab — also found large variation in how deeply immune cells had infiltrated the various tumors and where different immune cell types, such as T cells or macrophages, assembled. Some metastatic tumor samples showed the cancer breaking through immune cell boundaries to continue the invasion of healthy tissue, perhaps illustrating a phenomenon called immune cell exhaustion, in which the immune system is overwhelmed by an aggressive cancer and can no longer contain its growth.
“If we can see exhausted T cells inside a tumor, we could potentially activate those T cells with a checkpoint inhibitor or other immunotherapies,” Ding said. “But if we don’t see them, we will know certain immunotherapies won’t work. These tumor maps can help us predict treatment resistance. We have never been able to talk this way about tumors before — being able to see that immune cells are present in the tumor, suggesting opportunities to exploit them for treatments.”
WashU Medicine researchers led two more studies as part of this package of publications. One, appearing in Nature Cancer and co-led by Ding and Gillanders, provides a detailed analysis of breast cancer, identifying how different types of breast tumors originate from different cell types. The research team also found that T cell exhaustion was common in an aggressive tumor known as triple-negative breast cancer. Knowledge of the “cell of origin” and the immune landscape in breast cancer could help guide future treatment strategies.
The other paper, appearing in Nature Methods and co-led by Ding, of WashU Medicine, and Raphael, of Princeton, describes new methods for 3D analyses of tumors, including those used in the study of the six tumor types that appeared in Nature.