$3.6 million to fund personalized 3-D brain maps to guide neurosurgeries
Academic-industry partnership aims to improve brain surgery
 Timothy Mitchell/Eric Young
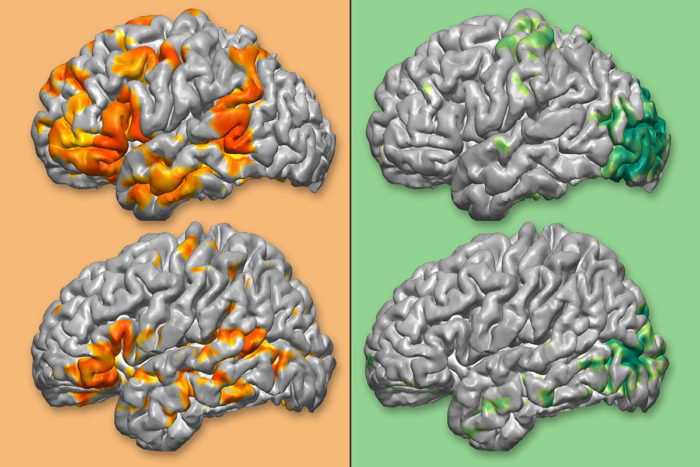
Timothy Mitchell/Eric YoungNeurosurgeons must avoid cutting into parts of the brain responsible for key functions such as language (orange) and vision (green), but individuals vary in where such functions are located (each of the top images compared with the bottom images above). Researchers are creating a software program that uses data from MRI scans to create personalized anatomic and functional brain maps and integrate them into a navigational system to guide physicians during neurosurgery.
Removing a brain tumor requires walking a fine line: Remove too little, and the disease remains; remove too much, and sight, speech or movement may be impaired.
To help strike that delicate balance, neurosurgeries often are performed with the aid of 3-D maps of patients’ brains. But such maps typically show anatomical landmarks and don’t indicate where critical brain functions such as language and motor function are found.
Now, a $3.6 million grant from the National Cancer Institute of the National Institutes of Health (NIH) will fund a collaboration between researchers at Washington University School of Medicine in St. Louis and Medtronic, maker of a neurosurgery navigational system that enables physicians to track where they are operating in relation to the patient’s brain anatomy. Together, the researchers will create a software program that uses information from MRI scans to build personalized 3-D maps of the location of brain functions, and integrates that information – along with an anatomic map – into a navigational system. These integrated maps can allow physicians to plan and perform surgeries more accurately and safely.
“Every neurosurgeon uses a navigation system, but we want it to be even better,” said Eric Leuthardt, MD, a professor of neurosurgery and of mechanical engineering and applied science, and the co-principal investigator on the grant. “We want to give them the ability not only to navigate the brain anatomy, but to know the implications of making incisions into each of those components of anatomy.”
When a part of the brain needs to be removed because of a tumor or other brain disease such as uncontrollable epilepsy, patients routinely undergo an MRI scan before the surgery to map the brain’s anatomy surrounding the portion to be removed.
However, mapping the functions those brain areas control is more difficult. The gold standard is cortical stimulation, in which doctors awaken patients during surgery and ask them to perform simple tasks – such as repeating a word – while they apply tiny electrical currents to the exposed surface of the brain. If the applied electrical stimulation interferes with a patient’s speech, the doctors know they have found a speech-related area of the brain.
But not everyone can be safely awakened during surgery, and some of those who can be awakened would really rather not be. Young children cannot undergo surgeries while awake or cooperate with the tasks. And the extent of damage to the brain caused by diseases such as brain tumors and epilepsy can make some adults unable to perform the tasks as well.
Leuthardt, with co-principal investigator Joshua Shimony, MD, an associate professor of radiology, and colleagues from neurosurgery and neuroradiology, have developed a technique to map functional areas of the brain in advance of surgery. The technique works on people of all ages and doesn’t require a patient to perform tasks.
Called resting-state functional MRI (rsfMRI), the technique relies on the fact that the brain is always active, even when a person is daydreaming, sleeping or even unconscious. You may not be moving, or even thinking about moving, but the left side of the motor area of your brain is busily communicating with the right. By identifying which parts of the brain are in communication, scientists can delineate functional networks.
“We have found a better way to create these functional maps, but even if we have them, the way functional information is handled can be very primitive,” Shimony said. “In many hospitals, the radiologist produces pictures of where on the brain the motor system is, where the language system is, where they are located relative to the surgical site, etc., but the information is not always well-integrated into the surgical navigation system.”
The NIH grant will allow Leuthardt and Shimony to integrate data from resting state functional scans into the Medtronic navigational system to make a 3-D structural and functional map of each patient’s brain.
A decade ago, Shimony and Leuthardt led a project – with the cooperation of Medtronic – to interface with the company’s StealthStation navigational system that is routinely used during neurosurgeries at Barnes-Jewish Hospital, where the two practice medicine. They set up the machine so it could take resting state functional data and produce individualized functional maps.
The system has reduced by one-third the number of surgeries at Barnes-Jewish performed while patients are awake and is popular among neurosurgeons there. But it requires a full-time employee with specialized expertise to analyze the data and help produce the functional maps.
The researchers reasoned that if resting state functional imaging were going to become a standard part of neurosurgical practice, it would be necessary to produce a user-friendly software program that does not require specialized training to operate. A key advance was made by MD/PhD student Carl Hacker, PhD, who figured out how to automate the analysis of resting state functional data so that it could be processed by an algorithm rather than an expert.
“We’re creating a software package that is going to combine our expertise in interpreting resting state data with the navigational technology at Medtronic, so that anyone who wants to use resting state MRI to map functional areas, or to make a brain map for use in surgical planning, can have that readily available,” Leuthardt said. “We think it will be a win-win situation.”






