$4 million funds study of sickle cell disease in teens, adults
Research to focus on improving outcomes for those with condition
 Ed Uthman
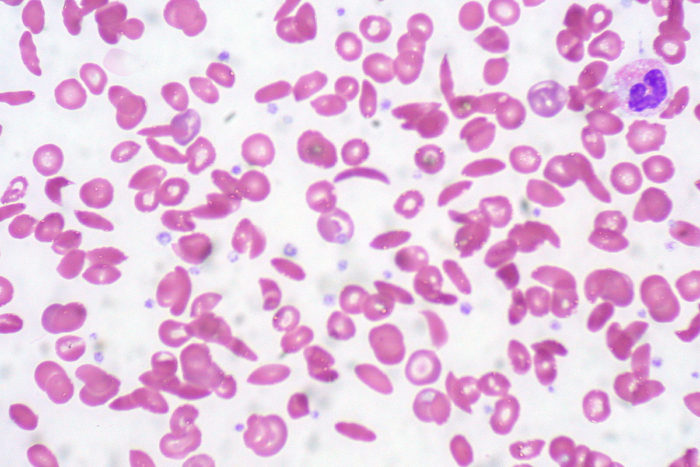
Ed UthmanIn sickle cell disease, red blood cells morph from round to crescent-shaped, or sickled, as depicted in this microscopic slide. The disease encompasses a group of inherited red blood cell disorders resulting from abnormal hemoglobin.
Over the past few decades, therapies for sickle cell disease have shifted this inherited blood disorder from its status as a fatal pediatric disease to a serious but manageable condition. But with the success come challenges for teens and adults living with a disease historically treated by pediatricians.
Allison A. King, MD, PhD, a highly regarded sickle cell disease researcher at Washington University School of Medicine in St. Louis, has received a six-year, $4.3 million grant from the National Institutes of Health (NIH) to further her investigations into the disease.
The funding is the first of its kind focused on improving health outcomes for teens and adults with the lifelong disease.
It is part of a larger effort spearheaded by the National Heart, Lung, and Blood Institute (NHLBI) of the NIH, which has awarded a total of $36 million to researchers at eight sites. The grants are aimed at helping improve health care for teens and adults with sickle cell disease, a condition affecting 100,000 people in the U.S., particularly African-Americans.
“There is a lack of research on teens and adults with sickle cell disease,” said King, an associate professor of occupational therapy, pediatrics and medicine who treats children and young adults at St. Louis Children’s Hospital, Barnes-Jewish Hospital and Washington University. “While a few large studies have improved the care of children with sickle cell disease, very few have focused on teens and adults. The purpose of this grant is to determine how and where to provide the best care to teens and adults with the disease.”
Sickle cell disease encompasses a group of inherited red blood cell disorders resulting from abnormal hemoglobin, a protein that delivers oxygen in the body. The condition causes typically round red blood cells to become crescent-shaped, or sickled, and leads to chronic pain and fatigue, organ damage and reduced lifespans.
“One of the most challenging barriers to overcome in patients with sickle cell disease is transitioning from pediatric to adult health care,” said King, who also is an associate professor of surgery and a medical director at Siteman Cancer Center at Barnes-Jewish Hospital and Washington University School of Medicine. “Older patients with the condition may experience frequent visits to the emergency room, receive poor follow-up after hospital discharge and have limited access to medications that boost survival and lessen physical pain. Other hurdles are not as clear, but we hope to learn more so we can improve the quality of care for this population.”
Prior studies on children with sickle cell disease have shown that early diagnosis and continued medical treatment can reduce symptoms, contribute to enhanced well-being and, ultimately, prolong life, King said.
Scheduled to run for six years, the NHLBI grants are part of the Sickle Cell Disease Implementation Consortium project. With additional funding from the NIH’s National Institute on Minority Health and Health Disparities, the health agency has committed another $6 million for a data coordinating center in Research Triangle Park, in North Carolina, that will support the sickle cell disease project.
Gary A. Silverman, MD, PhD, the Harriet B. Spoehrer Professor and the head of the Department of Pediatrics, said King’s grant highlights her scientific acumen and reinforces the School of Medicine as a research and treatment leader in sickle cell disease. “It also distinguishes Allison King as a top national expert, particularly on how the condition affects teens and adults,” he said.






