$6.2 million to help develop gene therapy for HIV
Genetically engineered B cells could produce super-antibodies to HIV
 Curiel Lab
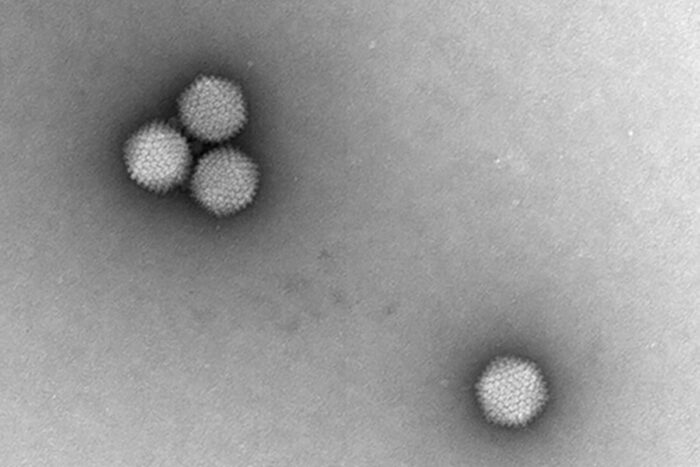
Curiel LabResearchers at Washington University School of Medicine in St. Louis have received a $6.2 million grant from the National Institutes of Health (NIH) to develop a gene therapy that would modify the immune system’s B cells to spur them to produce broadly neutralizing antibodies against HIV. In theory, such an approach could control or eliminate the infection without need for ongoing antiretroviral therapy. Shown is the engineered adenovirus designed to deliver HIV superantibody genes into B cells.
HIV infections can be controlled with medication, but such therapy must continue throughout patients’ lives because no strategy exists to eliminate the virus from the body or control the infection without ongoing treatment.
With the aim of developing such a strategy, researchers at Washington University School of Medicine in St. Louis have received a $6.2 million grant from the National Institutes of Health (NIH) to develop a gene therapy that would modify the immune system’s B cells to spur them to produce broadly neutralizing antibodies against HIV. In theory, such an approach could control or eliminate the infection without need for ongoing antiretroviral therapy.
“Permanent ways to control or eliminate HIV infection remain elusive, and their development is a major goal of the field,” said David T. Curiel, MD, PhD, the Distinguished Professor of Radiation Oncology. “The idea of modifying B cells — which naturally produce antibodies — to ensure that they manufacture specific antibodies that are broadly effective at targeting HIV is an exciting strategy. We have brought together a great team with expertise in HIV, gene therapy, and animal models of infection to work toward this goal.”
Curiel’s co-principal investigators are Michael R. Farzan, PhD, of Harvard Medical School and Boston Children’s Hospital, and Mauricio de Aguiar Martins, PhD, of the University of Florida.
Over the decades since HIV appeared, researchers have learned that about 1% of people with the virus are able to produce what might be considered superantibodies against the virus. Such individuals — known as elite neutralizers — can produce antibodies against multiple strains of HIV.
“Some people naturally have antibodies that can bind and destroy or deactivate very diverse strains of HIV, and we now have the ability to build those types of antibodies in the lab,” said Paul Boucher, a doctoral student in Curiel’s lab. “But just giving other patients these superantibodies is not an ideal solution, because these proteins would stay in the body only temporarily. Instead, our approach is to genetically modify the cells responsible for making antibodies — the immune system’s B cells — so they can always produce superantibodies against HIV whenever they may need to.”
Such engineered B cells could create, in theory, a state of permanent vaccination against the virus. Even if such a gene therapy doesn’t fully clear HIV from the body, the strategy could allow the amount of virus in the body to be controlled, keeping it at a minimal level and creating a functional cure, according to the researchers.
The strategy involves modifying a different type of virus, called adenovirus. When used in gene therapy, such viruses are genetically disabled so they can’t cause disease. The researchers then could engineer the adenovirus to carry the gene responsible for manufacturing broadly neutralizing antibodies to HIV. In the same viral vector, they also could include genes responsible for manufacturing the CRISPR/Cas9 gene editing proteins. In this way, the gene therapy delivery vehicle would carry into the body both the antibody gene that will be edited into the B cell genome and the genes to build the molecular tools to carry out that editing.
Using a three-part targeting strategy, the researchers would design the adenovirus to deliver its genetic payload only to B cells, avoiding other cell types. They have developed ways to modify the virus so that it is targeted directly to a protein that is expressed on the surface of B cells and no other cell types. The researchers can further restrict the targeting by using genetic methods to ensure that the CRISPR/Cas9 proteins can only be manufactured when their genes are delivered into B cells. Finally, they have developed strategies to modify the adenovirus in a way that stops its natural tendency to accumulate in the liver.
This strategy to modify B cells is distinct from another adenoviral gene therapy approach to HIV treatment that is currently in clinical trials led by principal investigator Rachel M. Presti, MD, PhD, a professor of medicine in the Division of Infectious Diseases at Washington University School of Medicine. HIV is difficult to eliminate from the body because the virus integrates its genome into the DNA of the infected individual’s T cells. The strategy currently in clinical trials is focused on using precise targeting of the CRISPR/Cas9 gene editing proteins to excise the virus from the genomes of all of a patient’s infected T cells. This strategy is being tested in a first-in-human, phase 1 clinical trial to determine its safety and preliminary efficacy at various doses.
Curiel said engineered B cells are ripe for developing new therapies to treat a wide variety of diseases. In November, a genetically engineered B cell therapy was administered to a patient for the first time at the University of Minnesota Medical Center. In that case, the therapy was designed to treat mucopolysaccharidosis type 1, a life-threatening condition in which the body lacks an enzyme necessary to break down large sugar molecules inside cells.
“Gene therapy with engineered B cells is an exciting new area of research,” Curiel said. “We look forward to combining our expertise in adenovirus gene therapy, HIV infection and preclinical models of disease to realize our plan for developing an HIV therapy that we hope can permanently control the infection.”






