Adding anti-clotting drugs to stroke care ineffective, clinical trial finds
Medications thought to show promise did not improve patients’ outcomes
 TIM MILLER
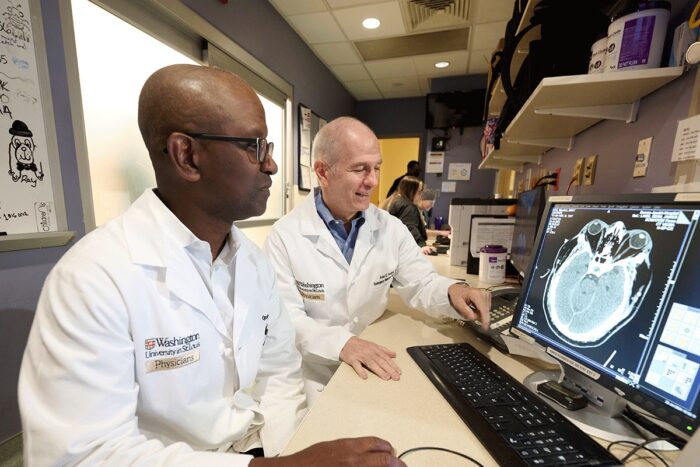
TIM MILLEROpeolu Adeoye, MD, and Peter Panagos, MD, (right) both professors of emergency medicine at Washington University School of Medicine in St. Louis, analyze a brain scan for stroke damage. Adeoye led a national clinical trial that found that two anti-coagulant medications are ineffective at improving post-treatment outcomes for stroke patients.
Stroke patients who survive a blood clot in the brain’s blood vessels are prone to developing new blockages during their recovery periods, even if they receive vessel-clearing interventions. In an effort to avoid further clots, doctors at 57 sites around the U.S. tested a possible solution: the addition of anti-coagulant drugs to medicine that dissolves blood clots.
But results from the clinical trial, led by Opeolu Adeoye, MD, head of the Department of Emergency Medicine at Washington University School of Medicine in St. Louis, indicate two such drugs did not improve outcomes.
The findings are available Sept. 4 in The New England Journal of Medicine.
“We’re a little disappointed in the results,” said Adeoye, who is also the BJC HealthCare Distinguished Professor of Emergency Medicine. “But it’s meaningful to optimal patient care that we’ve answered the question definitively. Neither of the drugs helps prevent further clots.”
The goal of the Multi-arm Optimization of Stroke Thrombolysis (MOST) clinical trial that Adeoye led was to test the efficacy of adding argatroban, a blood thinner, or eptifibatide, which inhibits blood platelets from sticking together, to the routine intravenous thrombolysis treatment.
The trial closed the chapter on this potential use of these medications, but Peter Panagos, MD, professor of emergency medicine and co-author on the study, said that efforts like these inform future advances in medicine, including potential new anti-coagulant treatments.
“Without negative trials, we would not know how to design new trials,” Panagos said. “Future success is built upon the hard work of previous research effort.”
Physicians do not have a lot of treatment options for patients who experience a stroke. Some patients undergo a procedure to remove the clot. Others receive intravenous thrombolysis to relieve the affected blood vessel through clot-dissolving medication delivered to the bloodstream. A number of patients receive both interventions.
“Even with those treatments, over half of patients still have a significant disability three months after their stroke,” said Adeoye, who treats patients at Barnes-Jewish Hospital and Missouri Baptist Medical Center and also provides stroke telemedicine consultation. “After you give the thrombolysis, the clot can re-form, which contributes to the stroke worsening or persisting.”
Preventing these clots with an additional treatment of anti-coagulant drugs seemed like a promising idea, especially as there are FDA-approved medications that earlier studies had suggested could be effective.
In the MOST trial, patients were randomly assigned to receive either argatroban, eptifibatide or placebo. Adeoye explained that the study had checkpoints built in to ensure that treatment outcomes were meeting efficacy thresholds in order to continue. The first checkpoint was set at 500 patients, which the team reached in 2023.
“When we looked at the data, it was readily apparent that neither drug was going to come anywhere close to our threshold,” he said.
In fact, the probability that either drug was helpful was less than 1%. Worse still, argatroban and eptifibatide were linked to greater incidences of disability and mortality within the three-month post-treatment observation window.
This correlation was not necessarily alarming; the safety monitors on the project found that the deaths appeared to have causes unrelated to the medications. The lack of improvement noted with the medications compared with what was noted with the placebo was reason enough to call off the trial.
There are more options to pursue in seeking to improve stroke outcomes. Adeoye said there are drugs in development that target different parts of the blood coagulating and clotting processes that may prove to be more effective than argatroban or eptifibatide, and other procedures such as direct arterial delivery through which such drugs might be more effective.
Panagos, who directs the new Section of Neurologic Emergencies in the Department of Emergency Medicine, added that WashU Medicine’s leadership in trials such as this one benefits the 1,700 stroke patients who are treated by WashU Medicine physicians at Barnes-Jewish Hospital every year.
“Because we are involved in and lead most of the key basic science and clinical research for stroke and cerebrovascular patients nationally and internationally, we can bring the latest interventions to our patients in St. Louis and help advance treatment and prevention strategies,” Panagos said. “Our involvement in clinical trials helps bring the highest quality, most innovative treatments to our community.”






