Artificial intelligence and the future of medicine
How big data could change health care
 Getty Images
Getty ImagesArtificial intelligence has the potential to transform medicine. Two Washington University experts, Philip Payne, PhD, and Thomas Maddox, MD, discuss how AI may change health care and what challenges need to be addressed before it can become part of routine care.
Washington University researchers are working to develop artificial intelligence (AI) systems for health care, which have the potential to transform the diagnosis and treatment of diseases, helping to ensure that patients get the right treatment at the right time.
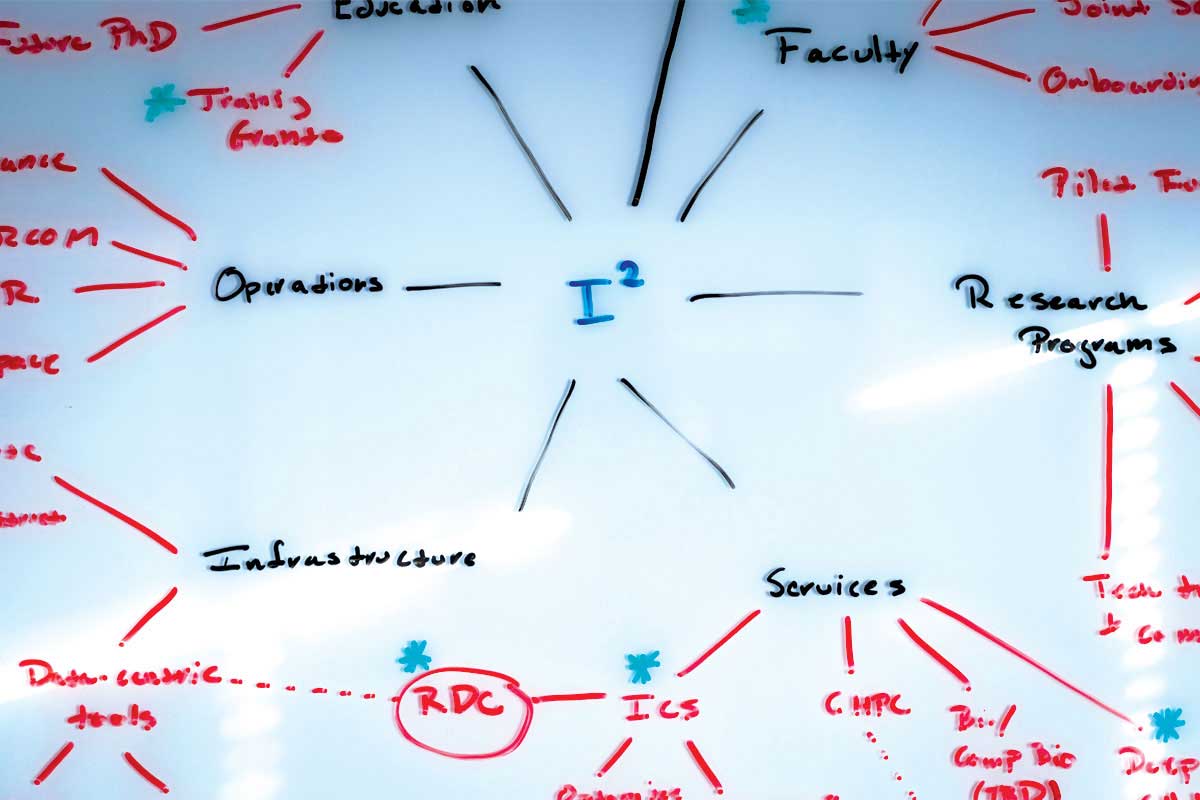
In a new Viewpoint article published Dec. 10 in the Journal of the American Medical Association (JAMA), two AI experts at Washington University School of Medicine in St. Louis discuss the best uses for AI in health care and outline some of the challenges for implementing the technology in hospitals and clinics. Philip Payne, PhD, is the Robert J. Terry Professor and director of the Institute for Informatics, and Thomas M. Maddox, MD, is a professor of medicine and director of the Health Systems Innovation Lab, launched in 2017 as a partnership between the School of Medicine and BJC HealthCare. The lab is aimed at developing innovative ways to deliver care and improve people’s health.
In health care, artificial intelligence relies on the power of computers to sift through and make sense of reams of electronic data about patients — such as their ages, medical histories, health status, test results, medical images, DNA sequences, and many other sources of health information. AI excels at the complex identification of patterns in these reams of data, and it can do this at a scale and speed beyond human capacity. The hope is that this technology can be harnessed to help doctors and patients make better health-care decisions.
Payne and Maddox answered questions about AI, including its capabilities and limitations, and how it might change the way doctors practice.
Where are the first places we will start to see AI entering medical practice?

Maddox: One of the first applications of AI in patient care that we currently see is in imaging, to help improve the diagnosis of cancer or heart problems, for example. There are many types of imaging tests — X-rays, CT scans, MRIs and echocardiograms. But the underlying commonality in all those imaging methods is huge amounts of high-quality data. For AI to work well, it’s best to have very complete data sets — no missing numbers, so to speak — and digital images provide that. Plus, the human eye is often blind to some of the patterns that could be present in these images — subtle changes in breast tissue over several years of mammograms, for example. There has been some interesting work done in recognizing early patterns of cancer or early patterns of heart failure that even a highly trained physician would not see.

Payne: In many ways, we already have very simple forms of AI in the clinic now. We’ve had tools for a long time that identify abnormal rhythms in an EKG, for example. An abnormal heartbeat pattern triggers an alert to draw a clinician’s attention. This is a computer trying to replicate a human being understanding that data and saying, “This doesn’t look normal, you may need to address this problem.” Now, we have the capacity to analyze much larger and more complex sources of data, such as the entire electronic health record and perhaps even data pulled from daily life, as more people track their sleep patterns or pulse rates with wearable devices, for example.
What effect will this have on how doctors practice medicine?
Payne: We think it’s important to emphasize that these tools are never going to replace clinicians. These technologies will provide assistance, helping care providers see important signals in massive amounts of data that would otherwise remain hidden. But at the same time, there are levels of understanding that computers still can’t and may never replicate.
Maddox: To take a treatment recommendation from an AI, even an excellent recommendation, and decide if it’s right for the patient is inherently a human decision-making process. What are the patient’s preferences? What are the patient’s values? What does this mean for the patient’s life and for his or her family? That’s never going to be an AI function. As these AI systems slowly emerge, I think we may start to see the roles of physicians changing — in my opinion, in better ways. Doctors’ roles may shift from being data collectors and analyzers to being interpreters and councilors for patients as they try to navigate their health.
Payne: That means we need to think about new ways to train physicians and other care providers as these systems come into medical practice. We want the humans in our health-care system doing the things that humans are uniquely suited to do, such as interpreting and counseling, as Tom described. And the computers in the system doing the things that computers are uniquely suited to do, such as collecting, filtering and analyzing large amounts of complex data. And those two things are complementary.
What regulatory issues — especially related to privacy — need to be addressed for AI?
Payne: As medicine is practiced now, there are moral, ethical and privacy contracts that already exist between health-care providers and their patients. If we can find a way to fully reflect those existing contracts from a technical standpoint, we’ll be in a good position. They provide guideposts.
Maddox: It’s an extension of the Hippocratic oath. There is privacy already inherent in the provider and patient relationship. Privacy requires two things: The first is the mechanics of protecting data, and the second is the establishment of trust. It’s incumbent on us to preserve that trust.
Payne: There’s a lot of talk about the ethics of data stewardship and whether there is a need for the equivalent of a Hippocratic oath for the people charged with protecting and using patient data appropriately. There is a moral and ethical contract that involves not only protecting patient privacy but making sure that information is used responsibly and in order to make the health-care system better. There’s a duty that people charged with doing so accept as part of their professions. Building systems to analyze data in health care is not the same as building systems that manage logistics when someone orders something online. The stakes are much higher, and it is important to acknowledge this difference.
Imagine AI is fully integrated into your practice. How might it change your day-to-day routine?
Maddox: I’m a cardiologist. Typically, patients I see include those who may have had a heart attack, or patients who are dealing with heart failure. Traditionally, we monitor these patients by having them come to our cardiology clinic for follow-up visits. For example, I might have a patient come and see me every six months. But this follow-up time period is basically chosen at random — there’s no specific medical reason for it.
With AI, in theory, I would no longer schedule these standard follow-up appointments. Instead, I would review the integrated, AI-analyzed, data streams of my thousand-patient practice every day. The AI algorithms would integrate multiple data streams that can paint a picture of my patients’ cardiac health on any given day. For example, I could see my patients’ activity levels measured by their wearable devices, their medication adherence patterns from pharmacy data, their breathing and pulse rates from their home-based sensors, their weight fluctuations from their “smart” scale, their exposure to air pollution from environmental sensors, and recent ER visits from their electronic medical record. Taking all that together, the AI could identify any patients who are at high risk for cardiac problems. From a heart-attack risk point of view, there might be a patient who is a smoldering fire, so to speak, and the system prompts me and my team to reach out to that patient for an appointment as soon as possible. For the remainder of my cardiac patients who don’t have any current high-risk features, then there would be no need for them to come to my clinic. We would just continue to monitor them remotely and be available for any problems.
Payne: What Tom just described is a smart health-care system — where the consumption of health care is driven by actual need. In his example, the AI sorted through a massive amount of different kinds of data and pulled out the one patient he needed to see and interact with. Some of the best ways to reduce health-care costs and improve health-care outcomes will be to eliminate the care that patients don’t need.
Right now, the challenges we need to address as we try to bring AI into medical practice include improving the quality of the data that we feed into AI systems, developing ways to evaluate whether an AI system is actually better than standard of care, ensuring patient privacy and making sure not only that AI doesn’t disrupt clinical work flow but in fact improves it. But if we do our jobs right and build these systems well, much of what we have described will become so ingrained in the system, people won’t even refer to it separately as informatics or AI. It will just be medicine.




 Related:
Related: 

