Atherosclerosis is Alzheimer’s disease of blood vessels, study suggests
Protein builds up as immune cells attempt to counteract plaque formation
 I. Sergin
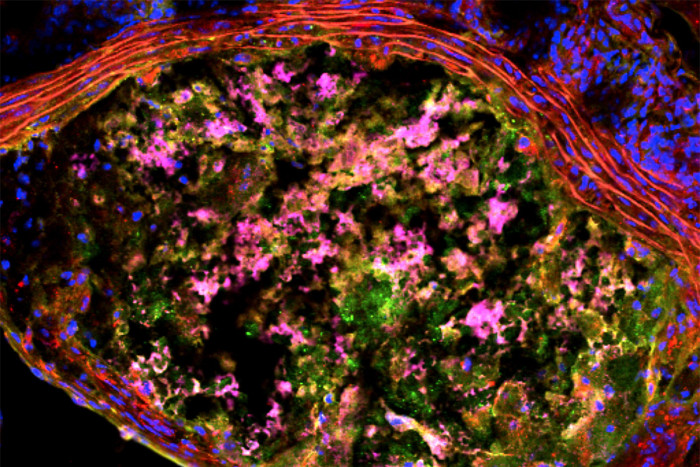
I. SerginA new study suggests that plaque forming in arteries has much in common with the progression of Alzheimer’s disease. The image shows a cross section of a mouse aorta, the main artery in the body, with a large plaque. Red lines near the top are the wall of the aorta. The plaque contains a dysfunctional buildup of immune cells called macrophages (pink) and protein waste (green).
In atherosclerosis, plaque builds up on the inner walls of arteries that deliver blood to the body. Studying mice and tissue samples from the arteries of patients, researchers at Washington University School of Medicine in St. Louis suggest this accumulation is driven, at least in part, by processes similar to the plaque formation implicated in brain diseases such as Alzheimer’s and Parkinson’s.
The study is published in the journal Science Signaling.
A look behind the scenes in the process of plaque accumulating in arteries, the new study is the first to show that another buildup is taking place. Immune cells attempting to counteract plaque formation begin to accumulate misshapen proteins. This buildup of protein junk inside the cells interferes with their ability to do their jobs.
Protein buildup is widely studied in the brain — accumulation of proteins such as amyloid beta and tau are hallmarks of Alzheimer’s, Parkinson’s and other degenerative neurological disorders. But until now, the process of misshapen protein buildup within cells has not been implicated in atherosclerosis.
“In an attempt to fix the damage characteristic of atherosclerosis, immune cells called macrophages go into the lining of the arteries,” said senior author Babak Razani, MD, PhD, assistant professor of medicine. “The macrophage is like a firefighter going into a burning building. But in this case, the firefighter is overcome by the conditions. So another firefighter goes in to save the first and is likewise overcome. And another goes in, and the process continues to build on itself and worsen.”
The researchers showed that this protein buildup inside macrophages results from problems with the waste-disposal functions of the cell. They identified a protein called p62 that is responsible for sequestering waste and delivering it to cellular incinerators called lysosomes. To mimic atherosclerosis, the researchers exposed the cells to types of fats known to lead to the condition. The researchers noted that during atherosclerosis, the macrophages’ incinerators become dysfunctional. And when cells stop being able to dispose of waste, p62 builds up. In a surprise finding, when p62 is missing and no longer gathers the waste in one place, atherosclerosis in mice becomes even worse.
Razani and his colleagues, including the study’s first author, Ismail Sergin, PhD, a postdoctoral research fellow, also found these protein aggregates and high amounts of p62 in atherosclerotic plaque samples taken from patients, suggesting these processes are at work in people with plaque building up in the arteries.
“That p62 sequesters waste in brain cells was known, and its buildup is a marker for a dysfunctional waste-disposal system,” Razani said. “But this is the first evidence that its function in macrophages is playing a role in atherosclerosis.”
The study demonstrates that p62’s role in gathering up the misfolded proteins is protective against atherosclerosis, even if the cell can’t actually dispose of the waste it gathers.
“If p62 is missing, the proteins don’t aggregate,” Razani said. “It’s tempting to think this might be good for the cell, but we showed this is actually worse. It causes more damage than if the waste were corralled into a large ‘trash bin.’ You can imagine a situation where lots of trash is being generated and see that it would be better to keep it all in one place, rather than have it strewn across the floor. You might have difficulty removing the trash to the dumpster, but at least it’s contained.”
In atherosclerosis, and perhaps in the brain disorders characterized by protein accumulation, such evidence suggests it would be better to focus on ways to fix the cells’ waste-disposal system for getting rid of the large protein aggregates, rather than on ways to stop the aggregates from forming.






