Brain rewires itself after injury ‘on the edge of what’s compatible with life’
Stroke suffered as newborn went undetected for 13 years
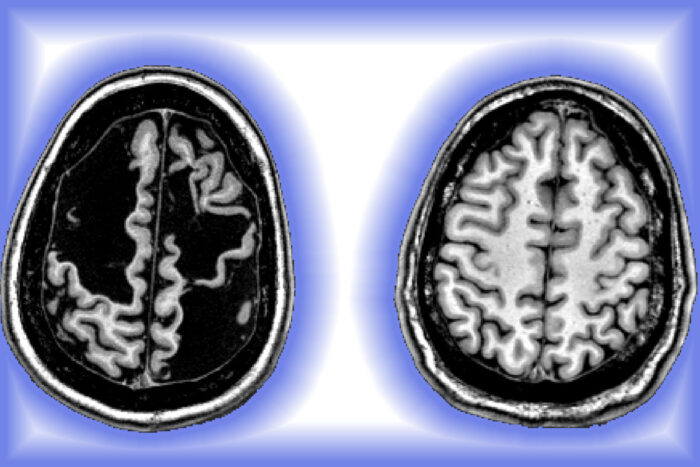 Photo courtesy of the Dosenbach lab
Photo courtesy of the Dosenbach labPictured is a high-fidelity image of Daniel Carr’s injured brain (left) compared with a typical brain, that of physician-scientist Nico Dosenbach, MD, PhD (right). The dark spaces in Carr’s brain reflect the significant loss of tissue in the parietal and frontal cortex in the right and left hemispheres. Despite the damage, Carr has lived a remarkably normal life. His case spotlights the brain’s remarkable resiliency to rewire itself, particularly early in life.
For 13 years, Daniel Carr had no idea he was missing part of his brain.
One of the first clues occurred on the baseball field. The coach of his seventh-grade boys’ competitive team in suburban St. Louis noticed Daniel’s unusual, albeit effective, fielding tactic in the outfield. Daniel wore his glove on his right hand. But if the ball headed toward him, he would take off his glove, catch the ball with both hands, throw the ball with his left hand and then put the glove back on his right hand.
“Let me tell you something about your son,” Kellie Carr recalled the coach saying. “Daniel can catch and throw a ball faster than most kids who do it the conventional way. He has the most incredible left hand. I’ve never seen anything like it.”
Shortly after that conversation, Kellie Carr began recalling her son’s other physical quirks. Her sister had noted that Daniel was sometimes clumsy when he tried to use his right hand. Further back, Kellie Carr recalled how, when Daniel was a year old, he walked unevenly, favoring his left side; it ended up being temporary and was soon forgotten. Also, Daniel had always been left-handed. That became evident when he was a baby, while for most children, hand dominance emerges around age 2 or 3.
Looking for answers, Kellie Carr took her son to a pediatrician, an orthopedist and a physical therapist. But no one could make sense of it.
No one, that is, until fall 2012, when the Carrs met “Dr. Nico” at Washington University School of Medicine in St. Louis. He delivered a preliminary diagnosis that made Kellie Carr’s jaw drop and heart race.
“I need to do more tests, but I think what’s going on here is that Daniel had a stroke when he was a baby,” Dr. Nico, formally known as Nico Dosenbach, MD, PhD, recalled telling her.
“A stroke?” Kellie Carr shrieked.
Indeed.
A stroke occurs when blood flow to the brain stops, depriving tissues of essential oxygen and nutrients. Small strokes often go unnoticed in infants, explained Dosenbach, an associate professor of neurology who treats patients at St. Louis Children’s Hospital. However, to confirm a stroke diagnosis, Dosenbach conducted a more extensive physical examination, including neuroimaging.
“It was the largest stroke I’d ever seen in a child who hadn’t died or suffered extreme physical and mental disability,” said Dosenbach, also an associate professor of occupational therapy, of pediatrics, of radiology and of biomedical engineering. “And yet, Daniel, who is now 22, has lived a remarkably normal life. His case spotlights the brain’s remarkable resiliency to rewire itself, particularly early in life. I knew Daniel’s brain justified further investigation.”
The research culminated in a case study published March 17 in The Lancet Neurology.
Daniel’s MRI scans revealed a large stroke had injured both sides of his brain when he was a baby. Further, dark spaces spanned parts of the cerebral cortex, the brain’s outermost layer and a central hub for thought, emotion, memory and higher-order functions. Those dark spots indicated significant loss of brain tissue, but Daniel didn’t seem to have cognitive, memory or emotional problems.
A bird’s eye view of Daniel’s brain showed asymmetric loss in both brain hemispheres of the motor cortex, which affects skills such as movement and balance.
The right side of a person’s brain controls movement on a person’s left side and vice versa. Most strokes target one side. But because a bilateral stroke damages both sides, the effects can be more serious.
“The extent of Daniel’s injuries may be on the edge of what’s compatible with life,” Dosenbach said.
With a confirmed stroke diagnosis, Dosenbach recruited Daniel, then 13 and with his mother’s consent, for research that would involve a battery of motor and neurobehavioral tests, and additional neuroimaging.
The research itself spanned six years. Dosenbach was a resident when he first met Daniel, and he faced many of the common hurdles confronting junior researchers, such as funding and time. But the biggest hurdle was finding someone who had the specialized skill set to analyze extensive neuroimaging data. Fortunately, Timothy Laumann, MD, PhD, now a fourth-year psychiatry resident at Barnes-Jewish Hospital, had the expertise.
Before they could begin the neuroimaging, Dosenbach and Laumann studied Daniel’s medical history, reviewing past doctor notes, bloodwork, and diagnostic tests and treatments.
The physician-scientists noted that as a newborn, Daniel had acquired an infection that lasted for three weeks. Doctors believed he had some kind of virus. Daniel experienced periods of distressed breathing, poor feeding, vomiting, diarrhea and persistent lethargy.
For about a week, Daniel was in a neonatal intensive care unit, where he received IV fluids and blood transfusions. However, diagnostic tests showed nothing that would indicate a stroke. Eventually, Daniel got healthy, went home and seemed to suffer no other serious problems.
“The risk of having a pediatric stroke greatly increases with a medical problem, especially an infection during the newborn period,” Dosenbach said. “However, usually there are more obvious signs that a stroke occurred. I can understand how no one suspected it.”
One out of 4,000 newborns suffers a stroke, according to the American Heart Association. Health outcomes vary, with about one quarter of the surviving babies having healthy motor and cognitive function, said Dosenbach.
“The brain can compensate more quickly and completely for strokes sustained in early childhood,” he said. “By contrast, large strokes in adults often cause death or severe functional impairment with little chance of recovery. However, the mechanics behind this are only beginning to be understood.”
Dosenbach and Laumann thought more might be revealed after a series of neurobehavioral tests. But for all, Daniel scored in the normal range. An assessment of his motor skills revealed a deficit in the right upper limb in strength, speed and dexterity relative to the left upper limb. However, everything else was developmentally typical.
Daniel underwent structural MRIs to examine his brain’s anatomy and pathology. Dosenbach and Laumann also used precision functional MRI mapping to understand how Daniel’s brain reorganized itself.
Such mapping entails repeated neuroimaging sessions to collect high-quality, detailed snapshots showing the unique complexities of a person’s brain. The scans measured Daniel’s brain during specific cognitive activities and when the brain was not actively engaged in tasks.
All told, Daniel spent about 30 hours having his brain scanned.
Daniel’s brain imaging data was compared with similar data from individual scans of other young adults, including Dosenbach, who has published several high-profile studies on data collected after scanning his own brain hundreds of times.
“Part of Daniel’s brain structure is gone,” Laumann said, in reference to their analysis of the MRI data. “He’s missing almost a quarter of his cortex.”
The dead tissue in Daniel’s brain forms hollows brimming with cerebrospinal fluid, a liquid that acts as a buffer for the brain, protecting it from injury while also circulating nutrients to tissue and removing waste products.
The neurons rewired to preserve brain functions. Connections emerged along islands of spared tissue, reviving motor and cognitive functions. Connections started anew in nearby neighborhoods of healthy tissues.
“Our findings illustrate the brain’s tenacity at reorganizing and recovering functions damaged by a massive stroke affecting both sides of his brain,” Dosenbach said. “Future studies of functional remapping relative to tissue loss may provide additional insights. Our results raise the possibility that variability in outcomes may depend on specific features unique to an individual’s brain.”
Daniel’s case also underscores the difficulties of accurate prognoses in early-life strokes. “Had Daniel’s brain injuries been detected when he was a baby, his family likely would have been told to expect severe developmental and cognitive delays. He may not have attended a typical school. He may not have played sports.”
Despite the limited use of his right hand, Daniel went to his neighborhood schools, hung out with friends and played baseball, soccer and football from kindergarten through high school. He earned an associate’s degree from a technical college and works five days a week rebuilding diesel pumps for trucks.
“His stroke still shocks me,” Kellie Carr said. “How could I have not known? But looking back, maybe it was better that way. I might have babied Daniel and been afraid to let him be a regular kid. Maybe the best thing for him was living normally.”
Daniel agreed: “I think about my right hand daily because I have to constantly think five steps ahead to figure out how to compensate for not being able to use it properly, like I did with the baseball glove. But the last thing I want is for people to act like something is wrong with me. I’m fine.”






