Cancer drug may help patients with severe asthma
Therapy targets immune cells driving lung inflammation
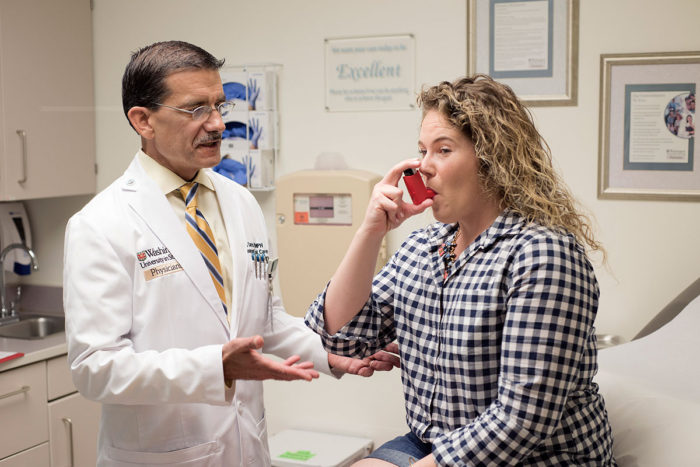 Robert Boston
Robert BostonMario Castro, MD, left, sees asthma patient Courtney Merlenbach in his clinic at Washington University School of Medicine in St. Louis. A new study Castro co-authored suggests a targeted cancer drug called imatinib (Gleevec) may help some patients with severe asthma who do not respond to standard therapy. Imatinib appears to reduce lung inflammation driven by a type of immune cell that responds to allergens.
A small clinical trial suggests that some patients with severe asthma may benefit from treatment with a targeted cancer drug. The study, conducted in part at Washington University School of Medicine in St. Louis, showed that imatinib (brand name Gleevec), commonly prescribed to treat chronic myeloid leukemia, also targets specific immune cells known to drive inflammation in the lungs.
The results are published May 17 in The New England Journal of Medicine.
“We are still in the early phase of this research,” said Washington University co-author Mario Castro, MD, the Alan A. and Edith L. Wolff Professor of Pulmonary and Critical Care Medicine. “The data are intriguing and promising, but we will need a much larger trial, perhaps with 300-500 patients, over a longer period of time, to see if Gleevec can have an impact on asthma symptoms and quality of life.”
The trial involved 62 patients treated at seven academic medical centers across the country and was led by Brigham and Women’s Hospital and Harvard Medical School. The researchers evaluated imatinib because it targets mast cells, which play a critical role in severe asthma.
“In asthma, mast cells are key inflammatory cells that react to allergens and cause release of histamine and other mediators of inflammation,” Castro said. “Those contribute to our patients’ symptoms, including bronchospasm — a sudden contraction of the walls of the airway — wheezing and shortness of breath.”
Castro said the trial was not large or long enough to determine whether patients experienced an improvement in symptoms, but the researchers did show that measures of airway inflammation were reduced in the patients receiving imatinib compared with a placebo.
The patients in the trial were randomly assigned to receive imatinib or a placebo. The patients, their physicians and those analyzing the data did not know which patients received the drug and which received the placebo. Patients took the assigned drug or placebo daily. The trial lasted six months, with measures of asthma severity and airway inflammation taken at the beginning of the trial and at the three-month and six-month marks.
Overall, patients taking imatinib performed better in assessments of airway reactivity and obstruction than patients receiving placebo. The improvement was modest, reaching statistical significance, but showing little evidence that clinical asthma symptoms had improved over the six months of the study.
The researchers also measured lower blood levels of a chemical called tryptase in patients receiving imatinib compared with placebo. Tryptase is produced by mast cells, with lower amounts of it suggesting the drug is reducing inflammation mediated by this type of immune cell.
Common treatments for asthma include inhaled steroids, which reduce all inflammation in a nontargeted way. In severe asthma, the steroid treatments often don’t control symptoms and the drugs have many side effects, especially for patients who have been taking them for many years.
“A lot of patients with severe asthma have been taking high-dose steroids since childhood, and this long-term use has many negative consequences,” Castro said. “These patients are developing conditions like obesity, diabetes, high blood pressure and osteoporosis from their steroid use. And the steroids are not even effective in controlling their severe asthma.”
Castro said the risks of taking a drug typically used for certain types of leukemia may be appropriate for patients with severe asthma if the drug provides the benefit of reducing or stopping steroid treatments. Though imatinib has a good safety record, it still raises concerns about suppressing the immune system. One patient stopped the trial because the white blood cell count became too low.
Patients in the trial taking imatinib and placebo experienced similar numbers of adverse events, with adverse events due to asthma more common in the placebo group. Patients taking imatinib were more likely to experience muscle cramps and low blood phosphate levels. Three patients taking imatinib reported a total of seven severe adverse events. Five patients taking placebo reported 10 severe adverse events. When asthma-related adverse events were not counted in this total, there were five events reported in the imatinib group and three events in the placebo group.






