Cancer treatment lessons from Hurricane Maria
Radiation oncologist discusses his colleagues’ struggles to treat patients after disaster
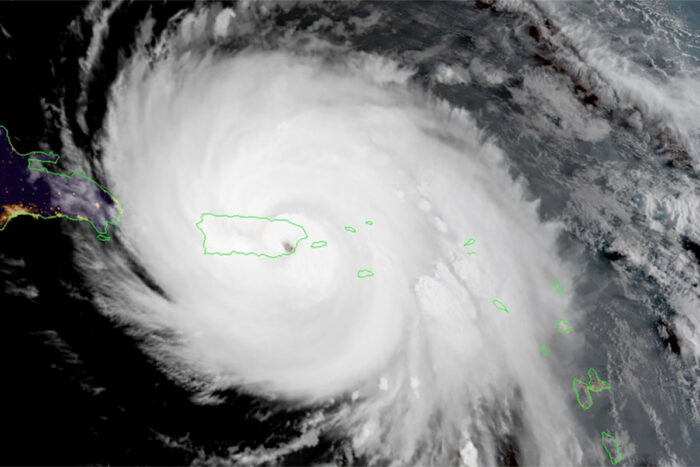 NOAA
NOAAHurricane Maria hit Puerto Rico on Sept. 20, 2017, devastating much of the island and its infrastructure. A radiation oncologist at Washington University School of Medicine in St. Louis is first author on a paper that focuses on how to prepare for such disasters, so that physicians who provide radiation therapy to patients have guidelines for what to do in advance, and how to recover afterward.
When Hurricane Maria churned across Puerto Rico on Sept. 20, 2017, it was the island’s second hurricane in less than two weeks.
More than 1 million residents were already without power because of a glancing blow from Hurricane Irma, which had ravaged nearby islands before going on to wreak havoc in Florida. Maria’s direct hit to the already fragile island was catastrophic. Extreme winds, torrential rains, flooding and landslides destroyed most of the power and telecommunications infrastructure in the storm’s path.
In the days following Maria, Puerto Rico native Hiram A. Gay, MD, an assistant professor of radiation oncology at Washington University School of Medicine in St. Louis, worked to contact family members, friends and his radiation oncology colleagues across the island. Despite the distance and erratic telecommunications, he was hoping to find some way to help.
 Related: Medical school physicians, staff aid hurricane victims
Related: Medical school physicians, staff aid hurricane victims
Liang, Char, Keeperman, Fehr, Davisson help in response to Hurricanes Harvey, Irma, Maria
Lessons that Gay and his colleagues learned from Hurricane Maria recently were reported in the journal Practical Radiation Oncology. The paper focuses on how to prepare for such disasters, so that physicians who provide radiation therapy to patients with cancer have guidelines for what to do in advance, and how to recover afterward. Recommendations include having clear methods of communication with staff and patients laid out in advance; providing portable data to individual patients about their own treatment plans so they may more easily receive care at a different clinic after the disaster; and following appropriate guidelines for how to compensate for missed radiotherapy sessions.
While the paper is specific to radiation oncology, some of the lessons may be more broadly applicable, especially since many of the problems were experienced throughout the island by all sorts of health-care providers, all of whom had to contend with loss of clean water, fuel, power and communication.
Gay, who is also a radiation oncologist at Siteman Cancer Center at Barnes-Jewish Hospital and Washington University School of Medicine, discussed disaster preparedness in the wake of Maria and lessons learned from the hurricane. Gay is the paper’s first author.
What did you learn from your colleagues’ experiences in Puerto Rico?
If you had shown me this paper before Hurricane Maria hit, I would have thought this level of preparation was overkill. But this massive catastrophe happened to people I know. Seeing how it affected my radiation oncology colleagues and friends was heartbreaking. The stress, challenges and anxiety they experienced is hard to imagine. They were trying to take care of their patients and families in a setting where there was a lack of power, fuel, potable water, and communications. Refrigerated food, gasoline, cell phones, internet, credit cards — things we take for granted — suddenly become a memory of a better past.
What happened in Puerto Rico was a worst-case scenario. Since it is an island, sending help poses many logistical challenges. It is less likely for mainland medical practices to experience this kind of widespread catastrophic failure — electricity, water supply, cell phone communications and internet. Still, we can learn from this experience about how to prepare for any kind of disaster, whether we’re talking about a major earthquake, hurricane, forest fire or other catastrophe. Even a cyber attack that brings down cloud computing systems, on which we are dependent for electronic charts and radiotherapy delivery, can bring our clinical work to a halt.
The authors on this paper shared how the hurricane affected them and what they learned, and a panel of experts contributed recommendations on how best to deal with gaps in therapy for lung, head and neck, uterine, cervix, breast and prostate cancers. Depending on the type of tumor and length of the treatment gap, many patients may require adjustments to their treatment to make up for lost time.
What happened in the early days right after the storm?
At first, it was just an exercise in trying to reach people. There are 18 radiation oncology practices in Puerto Rico, and some of them I wasn’t able to reach for months after the storm. I tried text messaging, email, landline phones. One radiation oncologist in Puerto Rico had to use a satellite phone. In some cases, it was easier for me to talk to different practices on the island than it was for them to contact each other, so I acted as a go-between. I called radio stations and helped spread messages to patients about which clinics were up and running. The community served by a radiation oncology practice in the town of Humacao, close to where hurricane Maria landed, was hard-hit. The staff went door to door trying to find their patients and were successful in locating all but one in the aftermath.
For a while, I tried to coordinate messages with the Federal Emergency Management Agency (FEMA) about which practices needed diesel fuel for their generators. The American Society for Radiation Oncology (ASTRO) was very supportive of all these efforts.
At first, the priority was survival. People were just securing food, water and shelter. Power loss to the island was total, so ATMs were not working. If you don’t have cash on hand, it’s hard to do anything. Some radiation oncology practices that were part of hospitals expressed some frustration because they felt like they could treat patients, but the hospital did not necessarily allocate emergency power to radiotherapy. It’s important for doctors to have a plan as to how the power generated by emergency diesel generators should be allocated in a crisis. There are many ethical implications that have to be carefully evaluated.
How did the practices prepare for the hurricane, and how could that preparation have been better?
In general, Puerto Ricans are quite familiar with hurricanes. I remember at least two from my childhood, and at the most, I missed two weeks of school until things went back to almost normal. But this one was different — the destruction was on a new scale. Because hurricanes are relatively common, pretty much all of the radiation oncology practices already had diesel generators. But these generators are not designed to run uninterrupted for months. With the total loss of the power grid, one practice had to rely on its generator for 140 days. That’s unheard of, but they had overdesigned their system and were well-prepared despite having most of their diesel stolen after the hurricane.
One of the most important pieces was establishing communication channels and planning ahead with backup methods. Everyone should know ahead of time how you will get messages to your own staff and to your patients about what is happening at the clinic and which clinics are open and which aren’t. Local radio stations and newspapers were very important. For staff, internet and social media became important — Skype, WhatsApp, Facebook Messenger and Zello are all options that should be considered if available. Often, it is a process of trial and error between landlines, internet, cell phones, satellite phones.
Have you received feedback on this work from medical providers in hurricane-prone areas?
Radiation oncology practices in the eastern United States are paying attention to what happened in Puerto Rico. The New Hanover Regional Medical Center Radiation Oncology group in Wilmington, N.C., which treats roughly 1,300 patients per year, was hit hard by Hurricane Florence in 2018 and couldn’t treat patients for almost a week. Aided by the findings of this paper, the radiation oncology practices in North Carolina will hold a meeting June 22 in Wilmington to discuss how to be better prepared for a natural disaster and minimize the impact on patients.
What message do you want to send to your fellow radiation oncologists and other health-care providers about disaster preparedness?
Radiation oncology is a highly technical specialty, relying on cutting-edge modern technology. Under normal circumstances, this results in excellent and precise radiotherapy. But this reliance on electrical systems and internet is a liability in natural disasters. If our machines and electronic medical record systems can’t communicate with the cloud, where patient data is stored and processed, the delivery of care may be compromised.
One recommendation the other authors and I suggest is that when we have advanced notice — and with a hurricane, there is usually some time to prepare — to give patients electronic copies of their own radiotherapy treatment plans and medical records on portable USB drives. Such thumb drives are pretty durable and make it easier for patients to be treated elsewhere if they have to move to another clinic after a disaster. If we are to continue treating patients with intermittent internet access or no access to our normal servers, we must have a way to bypass the cloud.
As we become more reliant on modern technology to deliver health care and as the intensity and frequency of storms increases driven by climate change, it’s important for health-care providers to consider worst-case scenarios and plan ahead for how they might deal with them to minimize the impact on our patients.






