Collaboration yields better view of Barrett’s esophagus
Washington University specialists have developed a powerful new tool to screen for Barrett’s esophagus, a condition where the esophagus lining is damaged
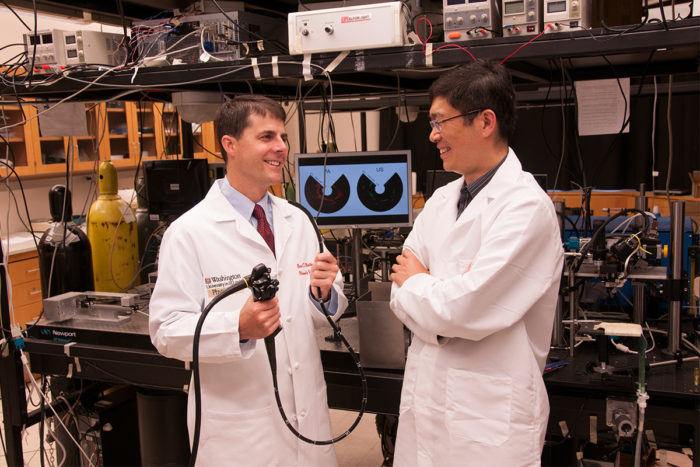
Photoacoustic endoscopy, invented by biomedical engineer Lihong Wang, PhD, right, may provide surgeon Brent Matthews, MD, a powerful new tool to screen for Barrett’s esophagus.
Barrett’s esophagus is a condition where tissue lining the esophagus is replaced by tissue similar to that lining the intestine. The condition increases the risk of developing cancer. It is measured in varying degrees or “grades” of severity, with high-grade patients having a higher risk of developing cancer than low-grade patients.
People diagnosed with Barrett’s esophagus must undergo surveillance using periodic endoscopic exams with biopsies. Because this technique may miss precancerous tissue, Brent Matthews, MD, chief of the Section of Minimally Invasive Surgery, was interested when Lihong Wang, PhD, the Gene K. Beare Distinguished Professor in Biomedical Engineering, contacted him about the possible use of a 3-D imaging method called photoacoustic tomography in the diagnosis of gastrointestinal disease.
“Once you have Barrett’s esophagus, you must undergo regular screening endoscopy for a lifetime,” says Matthews. “Biopsies every centimeter along the area where the Barrett’s is located are required. But there could be areas between the biopsy sites that actually could show a higher-grade Barrett’s esophagus, and you wouldn’t necessarily know that.”
New technology
Wang invented photoacoustic endoscopy, which applies photoacoustic tomography by way of an endoscope. With this technology, an endoscope pulses light into tissue, generating a sound wave that is then converted to an image. Wang and postdoctoral fellow Joon-Mo Yang, PhD, have been fitting a standard endoscope with the instrumentation to view the esophagus.
“There is a rotating mirror, which we spin to reflect light and sound,” says Wang. “We get a 360-degree perspective with dual contrasts, both optical and ultrasound. If there are lesions beyond one millimeter in depth, you cannot see them using standard optical endoscopy. In the current version, we can penetrate to about seven millimeters in depth.”
Photoacoustic tomography can also measure concentration and oxygen saturation of hemoglobin to assess blood vessel development and increased metabolic rates, respectively, which are hallmarks of cancer. The next step is to test the endoscope in animals, and ultimately to assess the technique in humans.
“Photoacoustic endoscopy could be a more accurate way to map out the esophagus as part of a surveillance program,” says Matthews.






