CRISPR enhances gene therapy to fight inherited diseases
Use of CRISPR and a virus extends life of genetic fix in mice
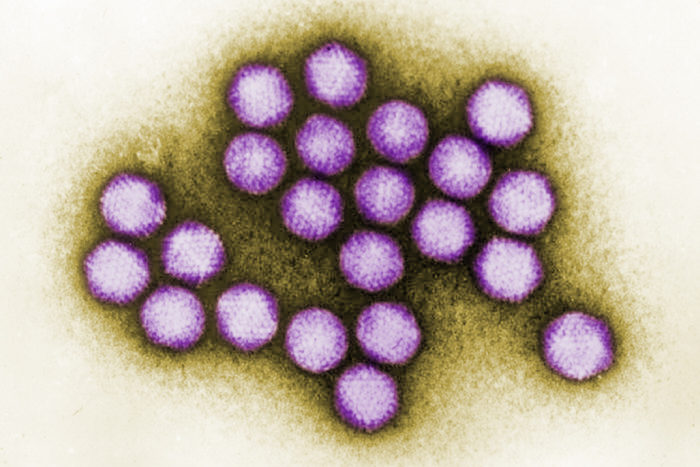 CDC/G. William Gary Jr.
CDC/G. William Gary Jr.Shown is a transmission electron microscope image of adenovirus particles. A new study, in mice, combined molecular tools — adenovirus and CRISPR — to improve gene therapy.
Gene therapy has shown promise in treating inherited genetic diseases, but a major issue that has frustrated scientists remains: Replacing a “bad” gene with a healthy one often is a short-lived fix. Typically, the healthy replacement gene works for just a few weeks.
Now, scientists at Washington University School of Medicine in St. Louis have combined the gene-editing tool CRISPR with a deactivated virus to deliver a healthy gene to a precise location in the bodies of living mice. More importantly, the researchers demonstrated that the inserted gene remained properly activated in mice for at least six months. The typical duration for this type of gene expression is four to six weeks, according to the investigators. The researchers ended the experiment at the six-month mark to study the mice, but said the length of sustained gene expression was equivalent to a fix that would last the lifespan of the mice.
The study is published online in the journal Gene Therapy.
“Over the years, one limit of gene therapy has been the difficulty in achieving long-term gene expression to treat disease,” said senior author David T. Curiel, MD, PhD, a professor of radiation oncology and cancer biology. “We have shown long-term expression of a gene that treats alpha-1-antitrypsin deficiency, which is the most common form of inherited emphysema. And now we’re applying this technique to hemophilia, a genetic condition in which blood does not clot properly.”
For decades, scientists have studied viruses for their potential to deliver genes directly into cells. After all, the common cold and other illnesses result when viruses infect cells and insert harmful DNA. To accomplish gene therapy, scientists have exploited this function of viruses, rendering them harmless and enabling them instead to deliver healthy genes to counteract disease.
For example, hemophilia patients lack a gene that orchestrates blood clotting, leaving them at high risk of dangerous bleeding. A recent study of 10 patients showed that a virus (without CRISPR) was successful in delivering the missing gene and helping mitigate the patients’ symptoms. But the technique remains a bit of a Hail Mary. Scientists have no control over where the virus inserts the gene into the cell’s DNA code, raising the risk of undesirable mutations.
But the advent of CRISPR gene-editing technology has changed that. While not perfect, CRISPR is a precise method to edit the genome and is user-friendly compared with other precision gene-editing techniques. It has been compared, for example, to the “find and replace” function of a word processor. Scientists tell CRISPR what combination of DNA “letters” to look for in a cell and what sequence of DNA to replace them with or to insert into that location. The challenge with CRISPR is delivering it to the right place inside the body.
Building on their own work and that of other groups, Curiel and his team have combined viral delivery methods with CRISPR to overcome the limits of both techniques. The researchers use adenovirus as the delivery vehicle and CRISPR as the navigator and the editor once it gets there, inserting the desirable gene into a part of the genome that is unlikely to cause problems.
“We targeted these viruses with CRISPR to a part of the genome that’s called a safe harbor,” said Curiel, director of the School of Medicine’s Biologic Therapeutics Center. “These are parts of the DNA sequence that are quiet, removed from more active areas, and where it’s unlikely for this type of editing to do anything harmful.”
To maximize efficiency and longevity, Curiel and his colleagues, including first author Calvin J. Stephens, a doctoral student in Curiel’s lab, used adenovirus as the delivery vehicle. A type of virus that can cause the common cold, adenovirus has been shown to be more efficient at gene transfer than other viruses.
Past work by another group involved a different type of virus to deliver CRISPR and a gene to correct an inherited disorder called Duchenne muscular dystrophy in a mouse model of the disease. Duchenne muscular dystrophy is caused when patients lack a protein vital for maintaining the structure of muscle.
According to Curiel, the virus used in the muscular dystrophy experiments — adeno-associated virus — is less efficient in delivering its cargo than the adenovirus used in the current study. Adeno-associated virus is difficult to produce and only can carry a small amount of DNA. While it was sufficient to correct for this type of muscular dystrophy, correcting for blood serum deficiencies requires much higher levels of gene expression. In other words, corrected muscle proteins stick around for a while, but serum proteins in the blood must be renewed constantly. To sustain this constant renewal, adenovirus was chosen because it can carry more cargo. But disadvantages of adenovirus include safety concerns.
The mice in this study appeared to be healthy for the duration of the experiment, but questions remain about the possibility of adenovirus, and perhaps the CRISPR protein machinery, triggering an immune response. Curiel and his team are further investigating the safety and efficacy of the combined adenovirus and CRISPR techniques, first in improving gene therapy for hemophilia.






