Cultivating gut microbes to shape health and treat disease
Groundbreaking work at Washington University School of Medicine is looking at ways our gut microbes affect our health
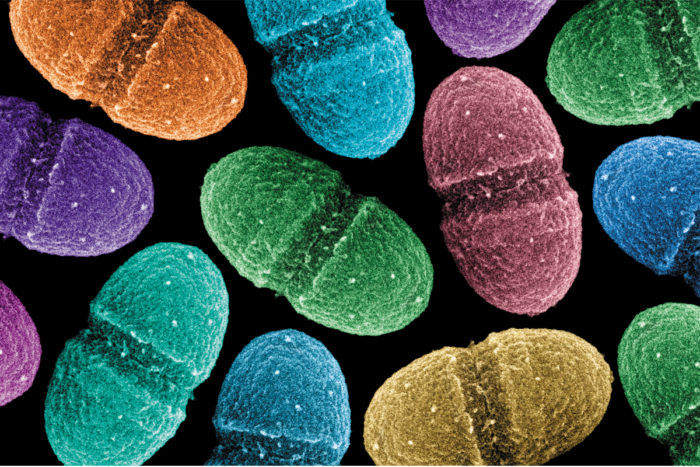
The microbe Enterococcus faecalis lives in the gut along with hundreds of other species that contribute to our health.
Our gut contains tens of trillions of microbes. They outnumber our own cells 10 to one. This community of microbes, known as the gut microbiota, affects us—for better and for worse—in ways scientists are now more fully appreciating.
On the positive side, these bugs are a key part of maintaining our well-being; not only do they help us absorb and make essential nutrients, they also boost our immune system and protect us against harmful pathogens. At the same time, they can contribute to many undesirable conditions, including inflammatory bowel disease (IBD) and irritable bowel syndrome (IBS).
Washington University faculty are conducting pioneering research related to how our microbiota shapes health and disease, defining what makes up a healthy gut, and understanding how to alter the gut microbiota to promote or maintain health. The work has global implications for addressing major human health problems, including obesity, malnutrition and possibly even brain disorders such as anxiety and depression.
Treating dangerous diarrhea
Scientists still aren’t sure what microbial mix makes up a healthy gut, but there are clearly some nasty bugs that, left unchecked, wreak havoc with digestion. One of these is the bacteria C. difficile, or C. diff, which can cause severe diarrhea.

“C. diff is virtually everywhere,” says Washington University infectious disease specialist Erik Dubberke, MD. “It’s been found in our homes, our drinking water, even our food.” The elderly and those in the hospital are particularly susceptible to this type of infection, which causes over 14,000 US deaths per year.
The main way many patients develop diarrhea associated with C. diff is through antibiotic use, which can destroy the good bugs that normally protect our guts from the infection this pathogen causes. Once C. diff has taken hold, it’s hard to get rid of; in up to 30 percent of patients, the infection recurs one or multiple times. And as many as 10 percent cannot get rid of these recurrent infections. To help these individuals, Dubberke’s lab is performing fecal transplants, which involve transferring fecal matter from a healthy gut to an infected gut. If all goes well, the healthy microbes take up residence, preventing the C. difficile from returning. To qualify for such treatment, patients who are referred to Dubberke first must meet strict criteria and have often exhausted all other forms of treatment.
Although such transplants are in some ways still the “Wild West,” says Dubberke, the scientific literature reports 80 percent to 85 percent success rates for stopping recurring infections. But Dubberke says there are still challenges: “We don’t yet have an ideal method for choosing donors, and we don’t know which bacteria are the best to use in the transplant.
He and his collaborators are working on identifying the most protective microbes and to commercialize preparation of pre-screened healthy fecal samples.
Radiation protection
Another way gut function can be disrupted is through radiation therapy for abdominal cancers.

“The epithelial cells that line the gut’s inner surface often get hit as ‘collateral damage’ during cancer treatment,” says gastroenterologist Matthew Ciorba, MD. When that happens, patients suffer from diarrhea, stomach pain and nausea—sometimes so severe they have to stop radiation therapy. The delay can compromise their cancer treatment.
In response to this potentially harmful chain of events, Ciorba and colleagues are evaluating whether probiotics, beneficial live bacteria taken in pill form, can protect intestinal cells and help patients complete radiation therapy with fewer side effects. So far, they have shown that the probiotic Lactobacillus GG (LGG) protects against radiation damage in mice. Their next step is to test LGG in humans. They plan to recruit 20 patients with rectal, pancreatic and anal cancers for an FDA-approved safety trial. Each study participant will receive the commercially available LGG probiotic Culturelle prior to beginning radiation therapy.
“Patients ask me every day what they can do and what they can take in terms of nutrition and wellness to help them through their cancer treatment,” says radiation oncologist Parag Parikh, MD, who is helping Ciorba run the trial at the Alvin J. Siteman Cancer Center at Barnes-Jewish Hospital and Washington University School of Medicine.* With this additional research, Parikh hopes to soon have the scientific evidence to recommend probiotics as an option for certain patients on radiation therapy.
Fighting obesity and malnutrition
Pioneering research led by Jeffrey Gordon, MD, director of the Center for Genome Sciences & Systems Biology at Washington University, is revealing an intimate connection among gut microbes, diet and nutrition. Studies performed by Gordon’s lab have shown that people who are obese have less diverse collections of microbes in their guts than those who maintain a healthy weight. The lack of certain microbes in obese gut communities may contribute to disease.

To investigate a potential relationship between the gut microbiota and obesity, Gordon’s lab recruited human twin pairs where one was obese and the other was lean. They transplanted gut microbial communities from each twin into germ-free mice. They found that mice receiving transplants from the obese twin developed obesity and metabolic issues, while mice receiving transplants from the lean twin did not. Next they repeated the transplants and placed the mice carrying the obese and lean microbial communities in the same cage. Microbes from the lean twin invaded the gut of the mouse with the obese twin’s microbes, preventing weight gain and metabolic problems. But this only occurred if the mice were given healthy human diets that were low in saturated fats and high in fruits and vegetables.
“Eating a healthy diet encourages microbes associated with leanness to quickly become incorporated into the gut,” says Gordon. “These findings are important as we look to develop next-generation probiotics as a treatment for obesity,” he adds.
Although some microbes may have an impact on making us too fat, others may contribute to the opposite problem—malnutrition, the leading cause of child mortality worldwide.
Our gut microbiota are established at birth and continue to change for the first three years of life. Gordon is leading an international team of scientists studying malnutrition in children from Malawi during those early years. Their work with 317 twin pairs finds that gut microbiota in malnourished children do not mature normally and may prevent some children from proper growth even when given therapeutic foods. The work suggests that successful treatment of malnutrition requires not only food-based therapies, but also long-lasting repair of the disrupted microbiota.
Microbial who’s who
A good deal of the research focused on the microbial communities and their genes–the microbiome–has concentrated on illness. But we still don’t know what bugs make up a healthy microbiota. Researchers at Washington University’s Genome Institute are gathering information on the species, genetics and function of the microbiota in our bodies; they hope to establish a baseline for health so they can then look for abnormalities associated with disease. Their studies include characterizing all the various types of microbes residing in the human body, including bacteria, viruses, fungi and other lower organisms.
“Our most immediate focus is to assemble a pipeline to complete microbiome projects more quickly,” says infectious disease genomics researcher Makedonka Mitreva, PhD, who is also assistant director at The Genome Institute. “Our ultimate goal is to use this information in the clinic to detect and trace outbreaks, and diagnose and treat patients with a wide range of health problems.”
Gut microbes and the brain
Often when we’re nervous, we feel the effects in our guts—that familiar ‘butterflies in the stomach’ sensation. So it’s not surprising that science is revealing links among our guts, gut microbiota and brain. “I think in many conditions such as anxiety and depression, a very logical place to look for answers is in the gut,” says Ciorba.
We have more nerve endings in the gut than in the brain. The gut is also home to 95 percent of the body’s serotonin—a hormone often associated with anxiety and depression. And studies suggest that gut microbes may alter the levels of many hormones that affect the brain.

Ciorba and his colleagues have shown that mice with gut inflammation show symptoms of anxiety and depression. His group is now researching IDO, an enzyme that is activated by gut microbes and interferes with serotonin production. Ciorba’s lab is looking at whether IDO may be a factor in the anxiety and depression often suffered by patients with inflammatory bowel disease. Studies of this pathway offer hope that certain dietary supplements that interact with the gut microbiota may help restore these hormones to healthy levels and alleviate these brain-related symptoms, says Ciorba.
It is still early days for this research, but the science so far has made it clear that our gut microbiota play a much bigger role in our health than we once thought. And whether it’s through fecal transplants, probiotics, diet or drugs, cultivating and nurturing our gut communities have become a key focus in the search for understanding disease and health.
*For more information about the probiotics and radiation therapy trial, please visit the trial site on ClinicalTrials.gov.






