Eczema drug effective against severe asthma
Dupilumab reduced asthma symptoms, improved lung function
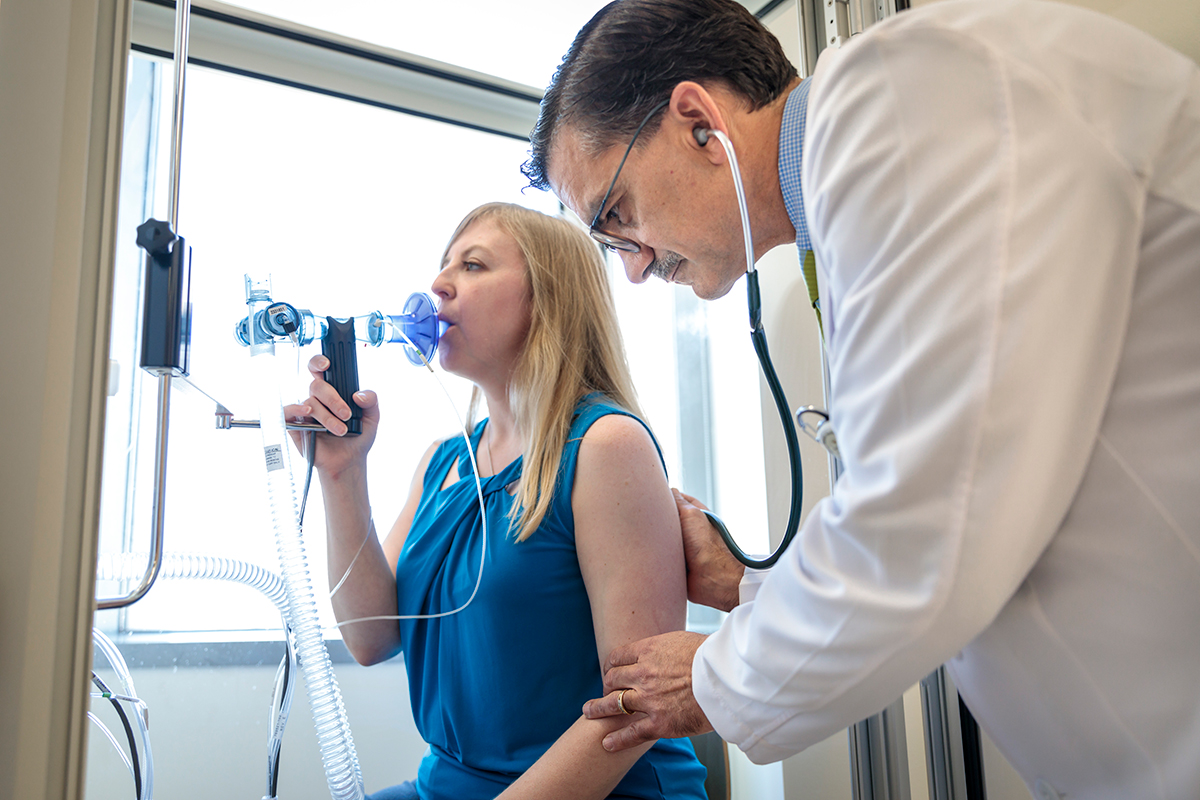
Huy Mach/Gaia RemerowskiTwo new studies of patients with difficult-to-control asthma show that the eczema drug dupilumab alleviates asthma symptoms and improves patients’ ability to breathe better than standard therapies. Researchers at Washington University School of Medicine in St. Louis and colleagues at other institutions conducted the studies.
Two new studies of patients with difficult-to-control asthma show that the eczema drug dupilumab alleviates asthma symptoms and improves patients’ ability to breathe better than standard therapies. Dupilumab, an injectable anti-inflammatory drug, was approved in 2017 by the Food and Drug Administration as a treatment for eczema, a chronic skin disease.
Researchers at Washington University School of Medicine in St. Louis and other institutions conducted the studies and were scheduled to present the results May 20 and 21 at the 2018 American Thoracic Society Conference in San Diego. The studies also will be published online May 21 in The New England Journal of Medicine.
The more than 2,000 patients enrolled in the studies suffered from moderate to severe asthma. All used standard asthma inhalers, and some also took oral steroids to control their severe asthma symptoms.
In one study, the rate of asthma exacerbations was almost cut in half for those taking dupilumab compared with those taking a placebo. On average, patients taking a placebo had close to one exacerbation per day during the year of the study. Exacerbations are periods of sudden worsening of asthma symptoms such as wheezing, coughing, shortness of breath and tightness in the chest.
Although the drug significantly reduced asthma symptoms for all patients, dupilumab worked particularly well in patients with high numbers of a specific type of white blood cell, called eosinophils, circulating in the bloodstream. For those patients, asthma exacerbations were cut by two-thirds.
“This drug not only reduced severe symptoms of asthma, it improved the ability to breathe,” said Mario Castro, MD, the Alan A. and Edith L. Wolff Distinguished Professor of Pulmonology and Critical Care Medicine. “That’s important because these patients have a chronic disabling disease that worsens over time with loss of lung function. So far, we do not have a drug for asthma that changes the course of the disease. Current drugs for severe asthma help reduce trips to the emergency room, for example, but they don’t improve lung function.”
The first study included about 1,900 patients of at least 12 years of age and with moderate to severe asthma requiring they use at least three different inhalers to control their symptoms. One inhaler contained a corticosteroid that reduces inflammation, another contained a long-acting bronchodilator that relaxes airway muscles, and the third was a “rescue” inhaler filled with albuterol, a short-acting bronchodilator that quickly opens up the airway in the event of a more severe asthma attack.
Patients taking these inhaled medications then were randomly assigned to receive either dupilumab or a placebo for one year. Patients receiving dupilumab — an injectable antibody — also were randomly assigned to a higher or lower dose of the drug. Neither patients nor their doctors knew whether they were receiving the drug or the placebo.
In addition to reduced symptoms, the patients receiving dupilumab showed improved lung function in a test of “forced expiratory volume.” This test measures the amount of air a person can force from the lungs during a deep exhale. Patients receiving dupilumab, regardless of dose, improved their lung function by approximately 130-200 milliliters greater than those receiving the placebo. In general, there were no significant differences between the patients receiving high and low doses of dupilumab.
Rates of emergency room (ER) visits and hospitalizations also were improved for patients receiving the drug. In the placebo group (with 638 patients), on average, 6.5 percent of the patients required an emergency room visit or hospitalization due to asthma during the study. In the dupilumab group (with 1,264 patients), on average, 3.5 percent of patients needed emergency care or hospitalization due to asthma.
Based on the second study, Castro said another benefit of the drug could be the ability to wean severe asthma patients off of chronic oral steroids, which can cause debilitating long-term side effects, including stunted growth, diabetes, cataracts and osteoporosis. The second study included about 200 patients using the same inhaled asthma medications as patients in the larger trial, plus additional oral steroids — usually prednisone — to control their more severe symptoms. Half of the patients receiving dupilumab in this study were able to completely eliminate prednisone use. And 80 percent of dupilumab-treated patients were able to at least cut their doses in half. Patients on placebo also reduced prednisone use but to a lesser degree, likely because the protocols of participating in a clinical trial help asthma control generally.
Castro said doctors would like to help patients rely less on steroids for asthma control because those with severe asthma can be forced to take these drugs for decades to enable them to breathe.
“I have patients who have had to stop working and go on disability because their asthma symptoms are so severe they can no longer function in the workplace,” Castro said. “I’m excited about the potential of dupilumab because I have so many patients who have maxed out on available therapies and they still can’t breathe. It can become a very disabling disease.”
Patients receiving dupilumab did experience known side effects of the drug, including pain and swelling at the injection site and a short-term bump in the number of eosinophil cells in the blood. Five patients who received dupilumab and three patients who received placebo died during the study period. According to the investigators and descriptions of these patients’ medical histories, all suffered from multiple severe medical conditions, and none of the deaths was deemed related to the study protocol.
 Matt Miller
Matt Miller





