Engineered immune cells help reduce toxic proteins in the brain
Study in mice points to a promising new approach for Alzheimer’s disease
 Getty Images
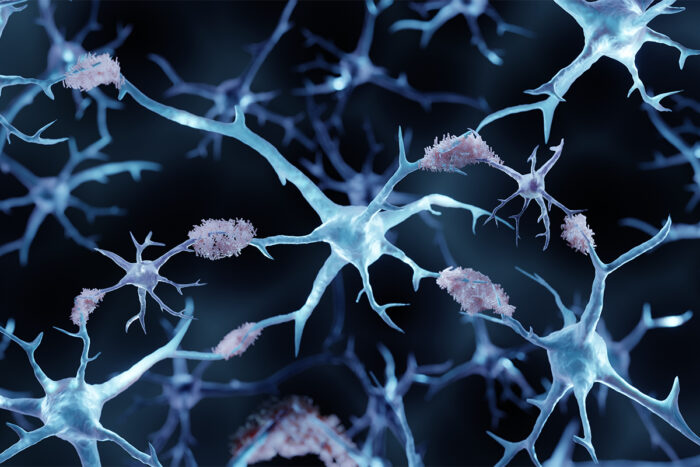
Getty ImagesResearchers at WashU Medicine and Weizmann Institute of Science designed a cellular immunotherapy that reduced amyloid beta plaques in the brains of mice.
Chimeric antigen receptor (CAR) T cell therapy, a type of immunotherapy that leverages the immune system to combat diseases, is a powerful treatment option for certain cancers. The treatment relies on genetically modified T cells — a type of immune cell — to destroy cancer cells.
Now, researchers at Washington University School of Medicine in St. Louis and the Weizmann Institute of Science (WIS) in Israel and their collaborators have applied a similar approach to treating neurodegeneration. They engineered CAR-T cells to target plaques of a key Alzheimer’s-causing protein in the brain called amyloid beta, offering a promising approach to treating the condition. In mice, they found that the engineered cells reduced the harmful amyloid plaques and improved the overall health of the brain tissue.
The study is published Feb. 9 in PNAS.
“We report the first CAR-T cell approach for a neurodegenerative disease,” said co-senior author Jonathan Kipnis, PhD, the Alan A. and Edith L. Wolff Distinguished Professor of Pathology and Immunology and a BJC Investigator at WashU Medicine. “It represents an exciting step towards finding novel therapies for Alzheimer’s disease. Equally exciting is the prospect of adapting these versatile cells to deliver therapeutic agents for different neurodegenerative diseases beyond Alzheimer’s, including amyotrophic lateral sclerosis (ALS) and Parkinson’s disease.”
Kipnis is an expert in the blossoming field of neuroimmunology, the study of how the immune system affects the brain in health and disease. A decade ago, Kipnis’ lab discovered a network of vessels surrounding the brain — known as the meningeal lymphatics — in mice and humans that drains fluid and waste into the lymph nodes, where many immune system cells reside and monitor for signs of infection, disease or injury. More recently, he and colleagues showed that T cells with neuroprotective properties can help with spinal cord recovery.
For the new study, Kipnis and his team collaborated with researchers led by co-senior author Ido Amit, PhD, a professor of immunology and the Eden and Steven Romick Professorial Chair at WIS, to leverage T cells to remove amyloid plaques from the brain. A year ago, WashU Medicine and WIS announced the launch of a collaboration to support joint research projects, such as this one.
Pavle Boskovic, PhD, a postdoctoral fellow in the Kipnis lab and the study’s first author, removed T cells from a healthy mouse and genetically modified them to recognize and respond to amyloid proteins in the brain. They injected the modified T cells into 6-month-old mice that had amyloid beta plaques in their brains. The mice, which carry genetic mutations found in Alzheimer’s patients, received three injections of the modified cells or non-modified cells spaced 10 days apart.
Ten days after the last injection, the researchers found a greater reduction of amyloid beta plaques in brains of mice treated with engineered CAR-T cells compared to those given control T cells. Additionally, CAR-T cell-treated mice had healthier brains compared to mice given control T cells, with the former experiencing a greater reduction in the activation of two brain cells called microglia and astrocytes. Such reduction in activation of these cells follows plaque reduction.
“In future research, we will explore how our engineered CAR-T cells improve brain health in Alzheimer’s disease,” Boskovic said. “We also aim to explore using them in mouse models of other neurodegenerative diseases that feature inflammation, with the hope that one day such cells can be safely and effectively used as a therapeutic to help people impacted by neurodegenerative disease.”
The study is Kipnis’ first project funded by the Carol and Gene Ludwig Initiative in Neuroimmunology Research, a grant from the Carol and Gene Ludwig Family Foundation supporting WashU Medicine research on neuroimmunology and neurodegeneration, with the goal of developing new treatments for Alzheimer’s disease.






