For children, young adults with recurrent AML, immunotherapy shows promise
Natural killer cells could help young patients with few treatment options
 Gara Elizabeth Photography
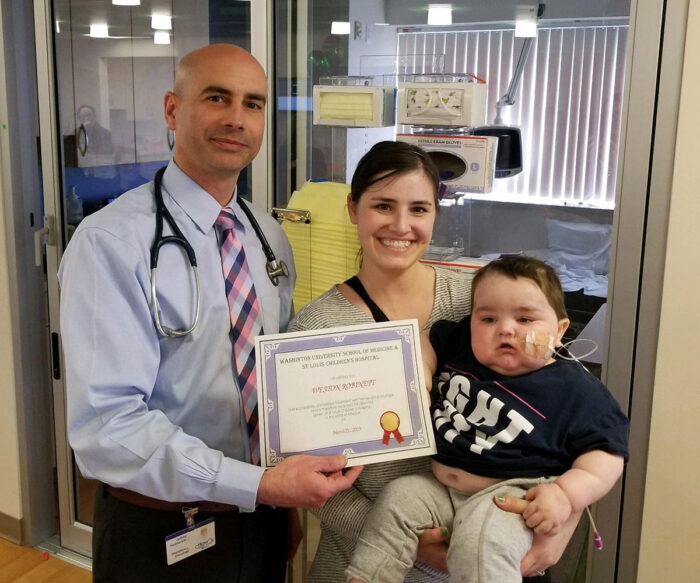
Gara Elizabeth PhotographyResearchers at Washington University School of Medicine in St. Louis have shown, in a small clinical trial, that pre-activated natural killer cells can help some children and young adults with recurrent AML and few other treatment options. Pictured is Weston Robinett, 3, a patient who received this investigational therapy at Siteman Kids at St. Louis Children's Hospital and Washington University School of Medicine. He remains in remission more than two years after treatment.
An immunotherapy harnessing the immune system’s “natural killer” cells has proven effective in treating acute myeloid leukemia (AML) in some adults whose cancers return. Now, researchers at Washington University School of Medicine in St. Louis have shown, in a small clinical trial, that the same natural killer cells also can help some children and young adults with recurrent AML and few other treatment options.
Results from the phase 1 trial, which included eight patients ages 1 to 30 years, are published online in the journal Blood.
“All of the patients enrolled in this study had very aggressive AML,” said first author Jeffrey J. Bednarski, MD, PhD, an assistant professor of pediatrics. “For all of them, their leukemia recurred after stem cell transplantation and was not responsive to several treatment regimens before they were referred to this study. This is a very challenging disease to treat — none of the patients had any curative options. The survival expectation for these patients was essentially zero. That three patients are still alive is very encouraging for this really challenging disease.”
Acute myeloid leukemia is a cancer of the blood and bone marrow that results in the overproduction of immature white blood cells, which crowd out healthy blood cells. Standard therapy involves chemotherapy and a stem cell transplant from a donor, which can result in a long-term remission. But for patients whose cancers return after stem cell transplantation, the disease becomes extremely difficult to treat, and most patients ultimately die from progression of their disease within a few months to a year.
Of the eight patients who received the investigational treatment, four achieved complete remission by day 28 after therapy. Two of the four stayed in remission for more than three months. One of these patients remains in remission today, more than two years after the treatment. Three patients who went into remission later relapsed. Of those three, two were able to receive a second stem cell transplant, and they’re still alive and doing well. Two other patients had a partial response to the therapy, in that their disease decreased, but they did not go into remission. The remaining two patients did not respond to the therapy.
“We found that the donor’s natural killer cells expanded, persisted and remained highly active against the leukemia in most of the patients for over three months,” said Bednarski, who treats patients in the pediatric cancer program at Siteman Kids at St. Louis Children’s Hospital and Washington University School of Medicine. “This therapy also was very well tolerated by the patients, who experienced almost no toxicities.”
 Robinett Family
Robinett FamilyNatural killer cells are a type of immune cell that attacks foreign or compromised cells, including bacteria, virus-infected cells and even cancer cells. Past work from Washington University researchers has shown that natural killer cells’ ability to attack cancer cells can be enhanced by exposing them to a specific cocktail of chemicals called cytokines. The natural killer cells are collected from a donor and then exposed in the lab to three cytokines called interleukins 12, 15 and 18. This exposure activates the cells and prompts them to remember this activation. When such “cytokine-induced memory-like” natural killer cells are given to the patient, they are more aggressive in attacking the cancer because of this pre-activation.
“A unique angle to this study is that we’re using the patient’s original stem cell donor’s cells to generate the memory-like natural killer cells, so the cells won’t be rejected by the patient’s immune system but are still able to fight the leukemia,” said senior author Todd A. Fehniger, MD, PhD, a professor of medicine who treats patients at Siteman Cancer Center at Barnes-Jewish Hospital and Washington University School of Medicine. “We’re also pleased to see evidence that these cells are extremely safe. They do not have the severe side effects that are sometimes seen in cellular therapies based on T cells. Using cutting-edge science within this trial, we also now understand these memory-like natural killer cells are very unique, even compared with conventional natural killer cells.”
Fehniger’s lab developed the methods for producing the cytokine-induced memory-like natural killer cells and led the original clinical trial of these cells in adults with AML.
Based on the experience of these eight patients, the investigators are making some changes to the protocol in an effort to make the treatment more effective for future patients. Bednarski said they will combine the memory-like natural killer cells with different chemotherapies to investigate whether that can optimize the killing of leukemia cells. They also will add a second infusion of the memory-like natural killer cells to extend the amount of time that the cells have to expand in the body and kill the leukemia cells.
“We plan to treat a larger group of pediatric and adult patients using this approach in an ongoing study,” Fehniger said. “Memory-like natural killer cells also are being explored as an experimental treatment for other cancers, including solid tumors such as melanoma and head and neck cancers, which are really exciting advancements in the field.”






