Immune system affects mind and body, study indicates
Immune cells produce molecule that influences vigilance, alertness in mice
 Kalil Alves de Lima
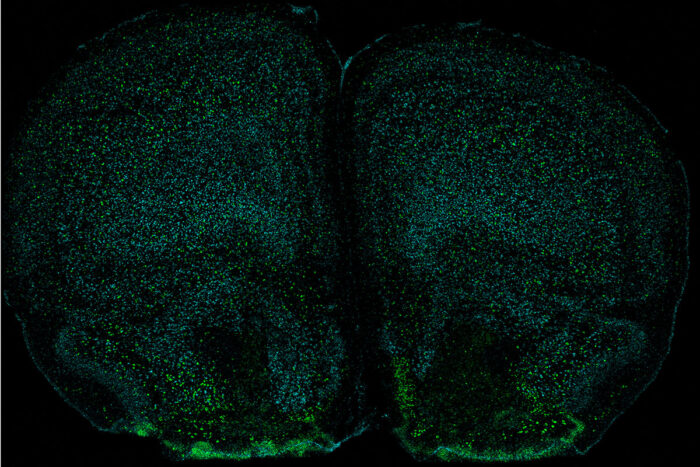
Kalil Alves de LimaNeurons (green) in a mouse brain have a receptor (cyan) that detects the immune molecule IL-17. Researchers at Washington University School of Medicine in St. Louis have discovered that a molecule produced by the immune system acts on the brain to change the behavior of mice.
New research at Washington University School of Medicine in St. Louis helps illuminate a surprising mind-body connection. In mice, the researchers found that immune cells surrounding the brain produce a molecule that is then absorbed by neurons in the brain, where it appears to be necessary for normal behavior.
The findings, published Sept. 14 in Nature Immunology, indicate that elements of the immune system affect both mind and body, and that the immune molecule IL-17 may be a key link between the two.
“The brain and the body are not as separate as people think,” said senior author Jonathan Kipnis, PhD, the Alan A. and Edith L. Wolff Distinguished Professor of Pathology and Immunology and a professor of neurosurgery, of neurology and of neuroscience. “What we’ve found here is that an immune molecule — IL-17 — is produced by immune cells residing in areas around the brain, and it could affect brain function through interactions with neurons to influence anxiety-like behaviors in mice. We are now looking into whether too much or too little of IL-17 could be linked to anxiety in people.”
IL-17 is a cytokine, a signaling molecule that orchestrates the immune response to infection by activating and directing immune cells. IL-17 also has been linked to autism in animal studies and depression in people.
How an immune molecule like IL-17 might influence brain disorders, however, is something of a mystery since there isn’t much of an immune system in the brain and the few immune cells that do reside there don’t produce IL-17. But Kipnis, along with first author and postdoctoral researcher Kalil Alves de Lima, PhD, realized that the tissues that surround the brain are teeming with immune cells, among them, a small population known as gamma delta T cells that produce IL-17. They set out to determine whether gamma-delta T cells near the brain have an impact on behavior. Kipnis and Alves de Lima conducted the research while at the University of Virginia School of Medicine; both are now at Washington University.
Using mice, they discovered that the meninges are rich in gamma-delta T cells and that such cells, under normal conditions, continually produce IL-17, filling the tissues surrounding the brain with IL-17.
To determine whether gamma-delta T cells or IL-17 affect behavior, Alves de Lima put mice through established tests of memory, social behavior, foraging and anxiety. Mice that lacked gamma-delta T cells or IL-17 were indistinguishable from mice with normal immune systems on all measures but anxiety. In the wild, open fields leave mice exposed to predators such as owls and hawks, so they’ve evolved a fear of open spaces. The researchers conducted two separate tests that involved giving mice the option of entering exposed areas. While the mice with normal amounts of gamma-delta T cells and levels of IL-17 kept themselves mostly to the more protective edges and enclosed areas during the tests, mice without gamma-delta T cells or IL-17 ventured into the open areas, a lapse of vigilance that the researchers interpreted as decreased anxiety.
Moreover, the scientists discovered that neurons in the brain have receptors on their surfaces that respond to IL-17. When the scientists removed those receptors so that the neurons could not detect the presence of IL-17, the mice showed less vigilance. The researchers say the findings suggest that behavioral changes are not a byproduct but an integral part of neuro-immune communication.
Although the researchers did not expose mice to bacteria or viruses to study the effects of infection directly, they injected the animals with lipopolysaccharide, a bacterial product that elicits a strong immune response. Gamma-delta T cells in the tissues around the mice’s brains produced more IL-17 in response to the injection. When the animals were treated with antibiotics, however, the amount of IL-17 was reduced, suggesting gamma-delta T cells could sense the presence of normal bacteria such as those that make up the gut microbiome, as well as invading bacterial species, and respond appropriately to regulate behavior.
The researchers speculate that the link between the immune system and the brain could have evolved as part of a multipronged survival strategy. Increased alertness and vigilance could help rodents survive an infection by discouraging behaviors that increase the risk of further infection or predation while in a weakened state, Alves de Lima said.
“The immune system and the brain have most likely co-evolved,” Alves de Lima said. “Selecting special molecules to protect us immunologically and behaviorally at the same time is a smart way to protect against infection. This is a good example of how cytokines, which basically evolved to fight against pathogens, also are acting on the brain and modulating behavior.”
The researchers now are studying how gamma-delta T cells in the meninges detect bacterial signals from other parts of the body. They also are investigating how IL-17 signaling in neurons translates into behavioral changes.






