Lung perfusion technology may increase the donor pool
Washington University surgeons are testing a new way of preserving lungs in hopes of increasing numbers of acceptable donors
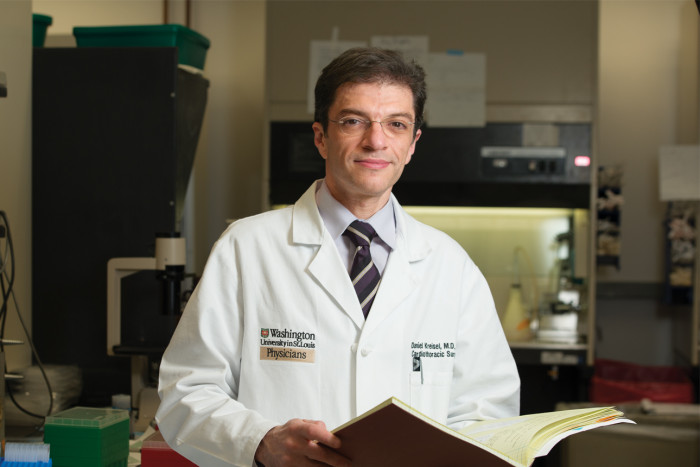
Washington University thoracic surgeon Daniel Kreisel, MD, PhD, is part of a team that is investigating lung immunology and transplantation.
In the 32 years since lung transplantation began, the demand for acceptable donor lungs has risen constantly, while the supply remains nearly unchanged. In fact, up to 25 percent of lung transplantation candidates die waiting for suitable donor organs. A new technology under investigation may broaden the pool of acceptable organs, potentially saving more lives.
Currently, donor lungs are harvested in less than 20 percent of multi-organ donors, primarily because of pulmonary edema, or fluid in the lungs. Before donor lungs are removed from the body, blood is drained from them, and they are perfused, or submerged, in a liquid solution formulated to preserve organ function.
Daniel Kreisel, MD, PhD, Washington University thoracic surgeon at Barnes-Jewish Hospital, is leading the Washington University portion of a multicenter clinical trial testing a technology called ex vivo lung perfusion in an attempt to rehabilitate lungs that are currently considered marginal into ones suitable for donation.
Lung perfusion circuit
In the trial, surgeons will remove marginal (less-than-optimal) donor lungs and place them on a circuit that includes a ventilator and heart-lung bypass machine to breathe into and perfuse the lungs using a specially developed protective solution that allows prolonged evaluation and stabilizes isolated lungs. While the lungs are on the circuit, the surgeons will assess the organs’ overall appearance and their function.
Ex vivo perfusion is already used in Canada and Europe and was recently approved by the U.S. Food and Drug Administration (FDA) as a Humanitarian Use Device. “At other centers, ex vivo perfusion has increased the volume of transplants by 15 percent,” says Kreisel. “Up to 50 percent of the lungs that are being placed on the circuit can be used.”
Washington University thoracic surgeons Varun Puri, MD, and Alexander Krupnick, MD, will join Kreisel in using ex vivo lung perfusion at a Mid-America Transplant Services facility dedicated to donor organ retrieval and located about 1.5 miles from Barnes-Jewish Hospital.
“At the end of three to four hours of perfusion, we decide whether these lungs are potentially transplantable or not,” says Puri.
Depending on the outcome of the trial, the company that supplies the lung perfusion circuit could apply for FDA approval of unrestricted use.
About 200 transplantations have been performed worldwide using the system.






