Medicare approves genetic test for solid tumors
Test can quickly identify treatable cancer mutations, guide precision therapy
 Matt Miller
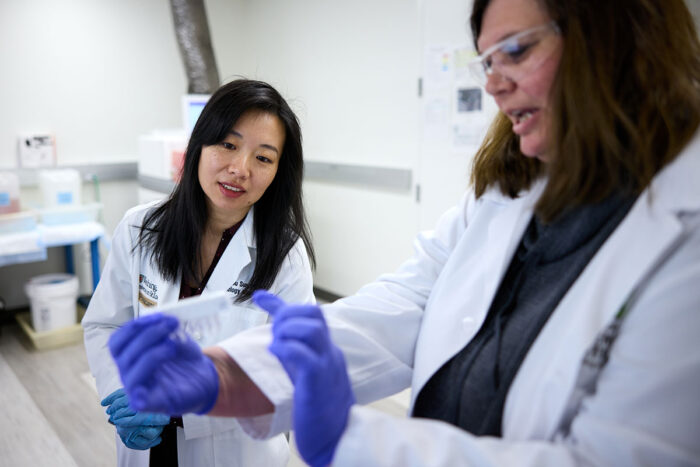
Matt MillerGatewaySeq, a genetic test that identifies cancer mutations in solid tumors and that was developed by researchers at Washington University School of Medicine in St. Louis, has been approved for reimbursement by the Centers for Medicare & Medicaid Services. Shelly O’Laughlin, (right) director of clinical operations for the Genome Technology Access Center at McDonnell Genome Institute, prepares the GatewaySeq test with Lulu Sun, MD, PhD, an assistant professor of pathology & immunology.
A genetic test that identifies cancer mutations in solid tumors and that was developed by researchers at Washington University School of Medicine in St. Louis has been approved for reimbursement by the Centers for Medicare & Medicaid Services (CMS). The test, known as GatewaySeq, identifies mutations that can be targeted with available drugs, helping advance precision medicine treatment strategies for patients with solid tumors, such as those of the lung, colon and pancreas.
GatewaySeq is the most recent genetic assessment tool developed by Washington University to receive CMS approval. Other recent such tests are ChromoSeq, which is a whole-genome sequencing test specifically for initial diagnosis of the blood cancers acute myeloid leukemia and myelodysplastic syndrome; and MyeloSeq, which is used to monitor the effectiveness of ongoing treatment for blood and bone marrow cancers, including acute myeloid leukemia, myelodysplastic syndrome and others.
Via Washington University Pathology Services, GatewaySeq testing is available at Siteman Cancer Center, based at Barnes-Jewish Hospital and Washington University School of Medicine. With the new approval of the test, doctors across the country who provide care for Medicare patients diagnosed with solid tumors also can order the test through Washington University Pathology Services. With Medicare approval for the test, Medicare will cover the cost.
“We designed this test to return results as quickly as possible to inform initial treatment decisions for most solid tumors,” said Eric Duncavage, MD, a professor of pathology & immunology and one of the test’s developers. “The test focuses on identifying known gene mutations that can help direct treatment when a patient is first diagnosed. This panel captures all of the gene mutations an oncologist needs to form a treatment plan for a newly diagnosed patient. If there is a drug approved by the Food and Drug Administration (FDA) that targets a specific gene mutation, that gene is on our test. We want to make this as accessible as possible so that every patient gets molecular testing to guide treatment from the beginning.”
The testing will be performed by the School of Medicine’s McDonnell Genome Institute, which has extensive expertise in genome sequencing and analysis. Scientists at the Genome Institute were the first in the world to demonstrate the validity of whole-genome sequencing in identifying genetic errors responsible for the development and progression of cancer.
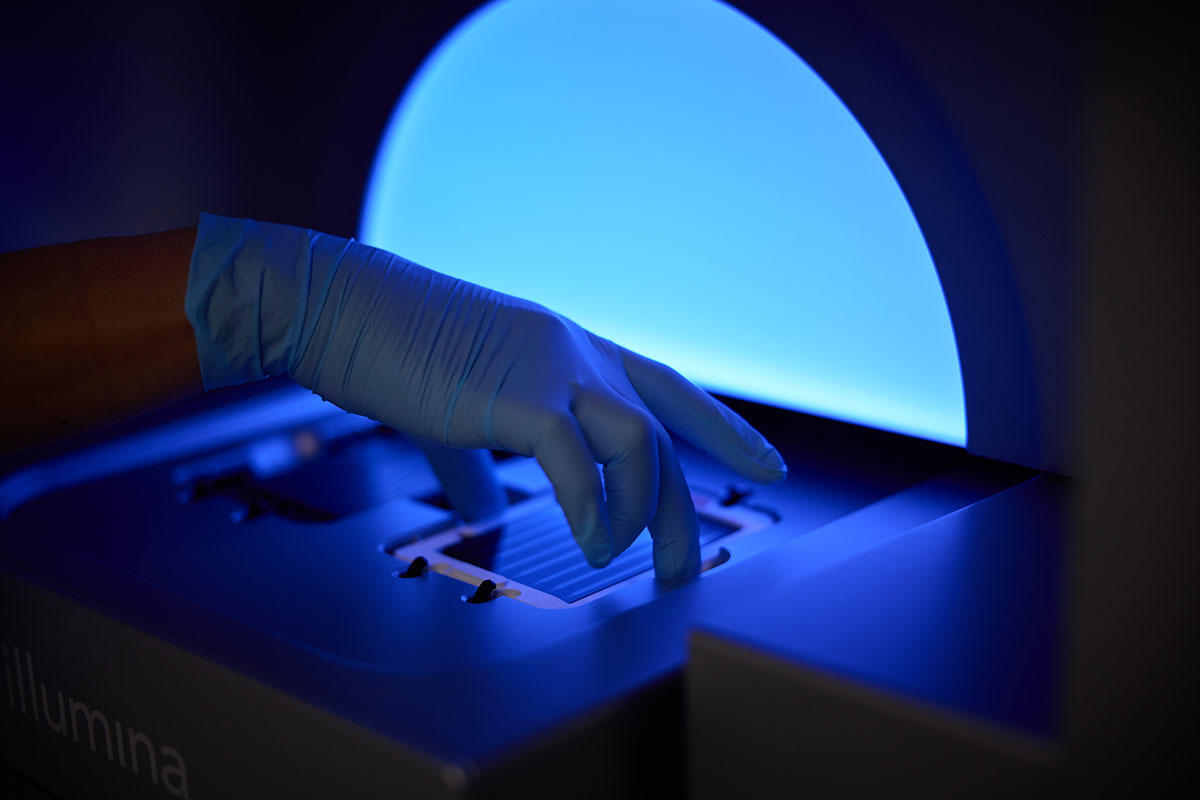 Matt Miller
Matt MillerThe test is designed to run on minimal DNA, according to Duncavage, making it easier to get a sufficiently sized tumor sample to return accurate results. By focusing on gene mutations that are treatable with FDA-approved drugs, the researchers could make the test return results faster and more cost effectively than other genomic tests, increasing accessibility. The researchers also prioritized speed in returning results so that patients whose tumors have druggable mutations can begin targeted therapy as soon as possible. Test results are available in 10 to 14 days, but Duncavage said the team plans later this year to reduce that time to seven to 10 days.
If the GatewaySeq test doesn’t find treatable mutations, doctors have the option of ordering additional genomic test panels that include more genes but may take longer to return results. Rather than identify specific drugs, other genomic test panels that include far more genes can inform care in other ways. For example, such tests can help determine how aggressive the cancer is likely to be, which can guide choices about surgery, radiation therapy and chemotherapy.
GatewaySeq can help guide treatment because of effective drugs now available for specific mutations that are common in solid tumors. For example, in certain types of lung cancer, a sizable number of tumors have mutations in a gene called EGFR, which can be treated with widely available EGFR inhibitors. A specific mutation in another gene called KRAS that is also common in lung cancer can be targeted with a drug approved by the Food and Drug Administration (FDA) in 2021. There is also a therapy available for gene fusions — where two genes fuse together and drive cancer — in the NTRK gene. The GatewaySeq test also can identify these fusions.
“NTRK fusions are not super common, but there are inhibitors that target that mutation, and they work pretty well, so it’s important to identify those patients,” Duncavage said. “In the past, because of limitations in time and cost, we might run molecular testing for only a handful of patients with solid tumors. We focused on those who had already received standard care but their cancers had returned or progressed. It was a last-ditch effort. Today, we can run this test on everyone in advance so we can identify the best treatment strategies as early as possible.”
Some of the tumors the GatewaySeq test can be used to analyze include cancers of the lung, breast, skin, brain, thyroid, gastrointestinal tract, genitourinary tract, gynecologic tract, hepatobiliary tract, bone and soft tissue, and lymphomas.
“The development of a genetic assessment tool for solid tumors represents a major step forward in our efforts to provide the most complete and up-to-date information crucial in a precision approach to treating these cancers,” said Richard J. Cote, MD, the Edward Mallinckrodt Professor and head of the Department of Pathology & Immunology, which runs the pathology service in collaboration with the clinical sequencing laboratory at the School of Medicine’s McDonnell Genome Institute. “These CMS approvals are a testament to the leadership of our department in developing tests that will specify the most precise treatments leading to the most optimal outcomes for our patients with cancer.”
Other co-developers of GatewaySeq include Lulu Sun, MD, PhD, an assistant professor of pathology & immunology, Drew Hughes, MD, PhD, an assistant professor of pathology & immunology, and David Spencer, MD, PhD, an associate professor of medicine and of pathology & immunology.






