New cell-based immunotherapy offered for melanoma
FDA approved treatment via Accelerated Approval pathway
 Getty Images
Getty ImagesWashington University physicians at Siteman Cancer Center, based at Barnes-Jewish Hospital and Washington University School of Medicine in St. Louis, will be among the first in the nation to administer a new cell-based immunotherapy to eligible patients with melanoma. Tumor-infiltrating lymphocyte therapy has received approval from the Food and Drug Administration for some patients with metastatic melanoma.
Siteman Cancer Center, based at Barnes-Jewish Hospital and Washington University School of Medicine in St. Louis, is one of the first centers nationwide to offer a newly approved cell-based immunotherapy that targets melanoma.
With the green light from the Food and Drug Administration (FDA), Washington University physicians at Siteman Cancer Center will administer tumor-infiltrating lymphocyte (TIL) therapy to treat certain adult patients with metastatic melanoma, an aggressive skin cancer that has spread to other parts of the body. The therapy is for patients with metastatic melanoma that can’t be treated with surgery and that has continued to grow and spread despite already having been heavily treated with other approved strategies, including chemotherapy and immune checkpoint inhibitors.
Washington University doctors and researchers were involved in clinical trials that led to the FDA approval.
The immunotherapy was approved under Accelerated Approval regulations, which allow the FDA to approve drugs for serious illnesses or conditions that have an unmet medical need. For approval, such drugs are shown to have an effect that indicates a likely clinical benefit to patients — for example, improving how they feel or function, or extending survival. The Accelerated Approval pathway generally gives patients the opportunity to access a promising therapy while further trials are conducted to confirm the drug’s clinical benefits.
Doctors, researchers and patients at Siteman also continue to participate in ongoing clinical trials investigating TIL therapy for patients with advanced lung and cervical cancers.
“These types of cell-based immunotherapies have been very impactful in blood cancers,” said George Ansstas, MD, an associate professor of medicine at Washington University and leader of the solid tumor TIL program at Siteman. “More recently, in the solid tumor area, particularly melanoma, we have seen progress in developing effective cell-based immunotherapies, and this is the first to be FDA-approved. While metastatic melanoma treatment was revolutionized with immune checkpoint therapy — the first immunotherapy for cancer — and many of our patients do very well, at some point most patients have some kind of recurrence. Now, we have another option to offer.”
Developed by Iovance Therapeutics, the new TIL therapy is called lifileucel (trade name Amtagvi).
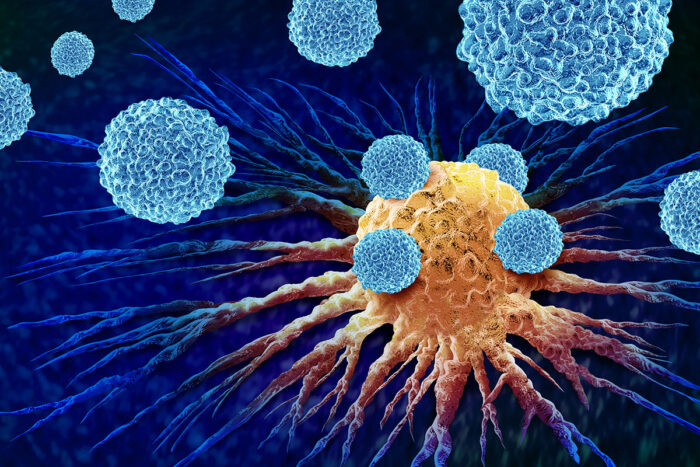
TIL therapy uses a patient’s own T cells that have already found and infiltrated the tumor in an attempt to kill the cancer. These natural cancer-killing immune cells can’t go it alone, though, because they are few in number and are quickly overwhelmed by the tumors.
“This is truly personalized cancer therapy, because the T cells are taken from the individual patient’s tumor,” said surgical oncologist Ryan C. Fields, MD, the Kim and Tim Eberlein Distinguished Professor, chief of the Section of Surgical Oncology and co-leader of the Solid Tumor Therapeutics Program, which is led by Fields and other Washington University physicians and researchers at Siteman. “These T cells are already targeted in multiple ways to the specific cancer cells. And because the T cells belong to the patient, there is no risk of the immune cells attacking the patients’ healthy tissues — a dangerous condition called graft-versus-host disease — as can sometimes happen with stem cell transplantation for blood cancers.”
The Cutaneous Oncology Program — within Washington University’s Division of Oncology and co-led by Ansstas, Fields and Lynn A. Cornelius, MD, the Winfred A. and Emma R. Showman Professor and director of the Division of Dermatology — will administer TIL therapy for eligible patients with melanoma.
For the therapy, doctors at an authorized treatment center take a sample of the tumor and send the tissue to an Iovance manufacturing facility, where tumor-infiltrating lymphocytes are isolated from the tumor and then expanded outside the body. This TIL therapy cell product is then cryopreserved and shipped back to the patient. When returned to the patient’s body via intravenous infusion, the tumor-specific T cells — now numbering in the billions — are much more effective at killing tumor cells throughout the body. Patients receive a course of chemotherapy to prepare the body to receive the T cells. Patients also are treated with interleukin-2, which boosts T cell activity.
According to the results of a clinical trial reported in The Journal for ImmunoTherapy of Cancer, in about 30% of patients, the tumors shrank at least 30%. And about half of the patients whose tumors responded to the therapy experienced a remission of at least 12 months following a single TIL treatment.
Treatment includes chemotherapy to eliminate existing T cells and create space for the new T cells to take hold and trigger a heightened immune response. This can result in a range of side effects, including increased risk of infection, internal hemorrhage, heart arrhythmias, respiratory failure, kidney failure and allergic reactions. Many of the side effects can be managed well, but some are potentially severe and life-threatening. With that in mind, the first centers to administer TIL therapy are those with extensive expertise treating patients with cell-based immunotherapies, such as CAR-T cell therapy for blood cancers.
For more information about TIL therapy, patients should visit siteman.wustl.edu or call 800-600-3606.






