New device offers advance in brain aneurysm treatment
Washington University physicians are using a new device that helps heal difficult-to-treat aneurysms with lower radiation exposure
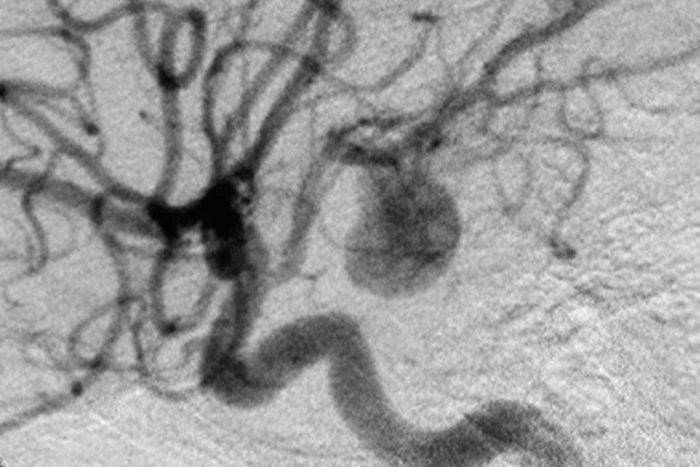
Cerebral aneurysm. Image courtesy of Wikimedia Commons.
A multi-center study has confirmed the safety and effectiveness of a new device for treating large cerebral aneurysms, blood-filled balloon-like bulges in the wall of a blood vessel in the brain. Known as the Pipeline™ embolization device, the stent helps the blood vessel seal off, allowing the aneurysm to heal and reducing the risk of bursting.
Barnes-Jewish Hospital was one of the trial sites and continues to be the major hospital in the region that uses Pipeline devices to treat aneurysms.
“This technology is changing the paradigm for treatment of many aneurysms,” said author Christopher Moran, MD, professor of radiology and of neurological surgery.
In some patients, aneurysms cannot be healed using the traditional methods of surgical clipping or coiling. If the neck of the aneurysm is particularly wide, physicians have to insert a stent to keep the coil from partially or completely slipping out of the aneurysm and into the blood vessel. Previously this was done with a Neuroform™ stent or an Enterprise™ stent, a cylindrical structure made of a metal mesh that lines the interior wall of the blood vessel.
Improved stent design
Pipeline stents are like these earlier stents, except that the meshwork that comprises the stent has significantly smaller pores, blocking blood flow through the stent and into the aneurysm. The design makes coil insertion unnecessary.

“The pipeline stent allows blood to clot over the neck of the aneurysm, which is followed by the development of fibrous tissue in response to the clot,” Moran says. “Finally the blood vessel regrows its interior lining and seals off the aneurysm, which naturally shrinks away and disappears.”
Both the pipeline stent and older procedures for treating aneurysms are performed using X-ray fluoroscopy, a technique that allows real-time viewing of a procedure using X-ray imagery and a contrast agent, or dye. But the pipeline stent can be inserted much more quickly than the peripheral stent, reducing radiation exposure.
After stent insertion, physicians have to carefully regulate inflammation and clotting. Patients take blood-thinners to ensure that clotting around the stent doesn’t take place too rapidly, potentially blocking the blood vessel and increasing stroke risk.
The study tracked 108 patients with difficult-to-treat aneurysms of the carotid arteries, which are the principal sources of blood flow to the brain. Surgeons placed stents in 107 of the patients. Six months after the surgery, the stents had successfully sealed off 78 of the aneurysms, for a success rate of 74 percent. Only six of the patients treated with the device had strokes or other fatal neurological events.
“The pipeline stent gives us a way to move from just filling the aneurysm to actually fixing the blood vessel. It also helps make treatment less risky by reducing patient radiation exposure,” Moran says.
Editor’s Note: Washington University radiologist Christopher Moran, MD, is a paid consultant for EV3, maker of the Pipeline embolization device.






