New insight into role of amyloid beta in Alzheimer’s disease
Studies hint at therapeutic strategies against devastating disease
 Robert Boston
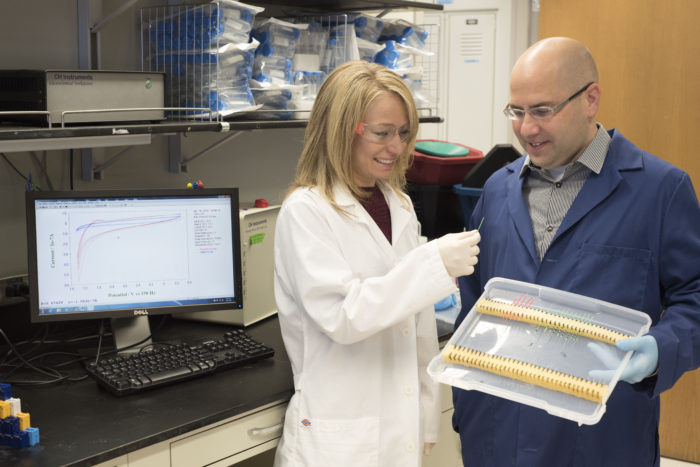
Robert BostonA new technique for measuring levels in the brain of amyloid beta, a key protein associated with Alzheimer’s disease, would help scientists design treatments to limit its accumulation. Carla Yuede, PhD, and John Cirrito, PhD, look at the tiny probe they used to measure the damaging protein.
New Alzheimer’s disease research details a technique that speedily measures levels in the brain of a damaging protein fragment, and insight into why mutations in a specific gene increase the risk of developing the disease.
Both studies, from researchers at Washington University School of Medicine in St. Louis, are available online in The Journal of Experimental Medicine.
The new measuring technique could lead to a better understanding of how amyloid beta, a key protein associated with Alzheimer’s disease, is produced in and removed from the brain, which would help scientists design treatments to limit the protein’s accumulation. Meanwhile, the genetic insight suggests that the brain’s own immune cells are crucial for containing the damage due too having too much amyloid beta.
When you use your brain – planning a meal, remembering the route to the store – your neurons release a sticky molecule known as amyloid beta, as a byproduct of their normal functioning. In healthy people, the protein fragment is cleared before it can do any damage. In people with Alzheimer’s disease, clearance is impaired, and amyloid beta builds up into clumps known as plaques.
Many of the treatments being studied for Alzheimer’s are designed to reduce amyloid beta in the brain. John Cirrito, PhD, an associate professor of neurology, Carla Yuede, PhD, an instructor in neurology, and colleagues have developed a new technique that measures minute-by-minute changes in amyloid beta levels in the brain. Previous techniques had allowed measurements only once an hour.
“For the last 14 years we had a technique in which we would do something to the mouse – give it a drug, have it perform a certain behavior – and we’d find out what happened to its amyloid beta levels an hour later,” said Cirrito, the senior author. “Waiting that long just wasn’t good enough. Neural activity happens on a rapid time scale, and we needed to see a direct connection between the intervention and the amyloid beta levels.”
In people, amyloid beta releases electrons when exposed to a small amount of voltage. These electrons can be measured as electric current, and the amount of current is directly proportional to the amount of amyloid beta.
The researchers attached antibodies that specifically detect amyloid beta onto a tiny electrode, zapped it with a small amount of voltage and measured the resulting current.
“People have used this approach for other molecules, but the detectors were the size of a microscope slide,” Cirrito said. “We adapted it into a five-micron fiber, which is way thinner than a human hair, so it could be implanted into the brain.”
Since mouse amyloid beta, unlike the human version, does not produce a current when exposed to voltage, the researchers used mice genetically modified to produce human amyloid beta. They treated the mice with a drug that blocked the production of new amyloid beta, and monitored how quickly the existing pool of amyloid beta disappeared.
The experiment revealed something surprising: One clearance pathway rapidly cleared amyloid beta at higher levels, but a different, slower one became dominant later as the levels dropped. These results contradicted research that Cirrito himself, among others, had published that suggested that the rate of clearance and the relative importance of the different pathways did not depend on the amyloid beta concentration.
“This is important if you’re devising a therapeutic strategy against Alzheimer’s disease,” said Cirrito. “If you hit the first pathway, you might have an effect quickly, but you may not be able to lower amyloid beta levels beyond a certain point. You’d have to consider targeting multiple pathways.”
Mutations increase risk
In a separate study, another Washington University team of researchers found that mutations in a specific gene increase the risk of Alzheimer’s by compromising the function of a cell that cleans up molecular debris.
People who carry a mutated form of the gene TREM2 have a fivefold increase in the risk of developing Alzheimer’s disease. The gene codes for a protein that, in the brain, is found only on a type of immune cell known as microglia.
“We found that microglia without TREM2 behaved abnormally,” said co-senior author Marco Colonna, MD, the Robert Rock Belliveau, MD, Professor of Pathology. “We speculate that in Alzheimer’s patients, over time, microglia fail to contain the accumulation of amyloid beta, which causes increasing damage to their brains.”

Microglia are the cleanup crew of the brain, engulfing and destroying dying cells, microbes and molecular debris, including amyloid beta. When TREM2 detects the presence of a kind of fat called phospholipids, it sends a signal that activates microglia.
To find out why losing TREM2 function raises the risk of Alzheimer’s disease, Colonna, co-senior author David Holtzman, MD, and colleagues knocked out the TREM2 gene in mice that have a genetic propensity to develop amyloid plaques.
In the brains of mice with TREM2, the microglia surround the amyloid plaques, but in those without TREM2, the microglia are dispersed. Without microglia hemming them in, the plaques spread out and markers of neuronal damage go up, although the total amount of amyloid beta stays the same.
“If you don’t have TREM2, the plaque spreads into the brain and destroys key parts of the neurons,” Colonna said.
Identification of the role of microglia in Alzheimer’s opens up possibilities for developing treatments. TREM2 is the first step in a molecular pathway that leads from detecting phospholipids to activating the cell. Microglia also bear inhibitory receptors on their surface, which send signals through a parallel molecular pathway to prevent the cell from being activated.
“You could target not just TREM2 but any molecule in the TREM2 pathway to make microglia more active,” said Colonna. “Or you could block any step in the inhibitory pathway.”
Another possibility is to have antibodies that act as a bridge between the plaques on one side and microglia on the other. In Alzheimer’s patients whose microglia do not surround the plaques on their own, such as those with defects in TREM2 or another molecule in the pathway, antibodies could bring the cells to the plaques.
Holtzman, the Andrew B. and Gretchen P. Jones Professor and head of the Department of Neurology, already is studying antibodies as a treatment.
“Now that we have shown how important microglia are, there are lots of things we can do to increase their function that might help,” Colonna said.






