New multiple sclerosis therapies help scientists understand roots of the disease
Washington University neurologists are working on finding new therapies to help patients with multiple sclerosis (MS)
Washington University neurologist Anne Cross, MD, remembers a very different world when she first began treating patients with multiple sclerosis (MS), an autoimmune disorder that affects motor function, almost three decades ago.
“It’s incredible—the MS clinic has changed so much,” says Cross, director of the John L. Trotter Multiple Sclerosis (MS) Center at Barnes-Jewish Hospital. “Throughout the first 10 years, we never had anything that was effective at slowing MS. But now we have an array of treatments either already in use, in clinical trials or on their way soon. It’s lots of fun to see so many new options opening up.”
Physicians normally group patients into one of four clinical subtypes to help anticipate the effects of MS and which medications may work:
- relapsing remitting
- secondary progressive
- primary progressive
- progressive relapsing
However, the unpredictability of MS continues to frustrate. The way patients respond to the new treatments, which have varied mechanisms of action, may provide scientists a much more accurate sense for what’s going wrong in the different forms of MS and in individual patients; that knowledge could lead to better, more targeted treatment and improved prognosis.
Current standard of care
Current medications offer some benefit for certain MS patients but fall short of controlling the disease. For relapsing remitting MS, the most common form, doctors currently often prescribe drugs such as beta-interferons or glatiramer acetate. But they must be taken as injections and can cause side effects including injection-site reactions and a flu-like illness. These factors may explain why up to 50 percent of MS patients treated with the drugs fail to regularly take their injections.
Additional oral medications are now becoming available for relapsing MS patients; they reduce relapse (“attack”) rate by about 30 percent to 50 percent, but it is controversial as to whether they reduce long-term disability. For secondary progressive MS and primary progressive MS, no treatments have proven effective to reduce progressive disability.
Newest options
The newest MS treatment to become approved by the FDA is teriflunomide, a compound that blocks rapid white blood cell growth—a key component of the autoimmune processes that cause MS. Teriflunomide is among the first MS drugs that can be administered orally via a daily tablet.
Another daily tablet, fingolimod, won FDA approval in 2010. It traps immune cells that contribute to MS inside the lymph glands where they develop and is effective for relapsing forms of MS. A multicenter trial called INFORM is ongoing to study whether fingolimod will also be effective as a treatment for primary progressive MS. Neurologist Becky Parks, MD, is leading that study at the Washington University/Barnes-Jewish Hospital site.
“There’s also evidence that fingolimod crosses the blood brain barrier and enters the brain and spinal cord,” Cross says. This may be helpful in MS since fingolimod binds to receptors in the brain, which leads to an increase in factors that may protect nerve cells in mice, she adds.
Fingolimod is now available as a treatment for relapsing forms of MS at Barnes-Jewish’s MS Center.
Emerging solutions
In addition to the INFORM trial, Washington University neurologists at the John L. Trotter MS Center are currently participating in three clinical trials of new monoclonal antibodies designed for MS treatment.
Robert Naismith, MD, is leading OPERA, an assessment of the benefits and risks of treating relapsing-remitting patients with a beta-interferon versus ocrelizumab, an antibody that depletes immune B cells. Cross is principal investigator for a second ocrelizumab trial, ORATORIO. This study is testing whether ocrelizumab will slow or stop neurologic progression in patients with primary progressive MS. Parks is leading the center’s study of daclizumab, an antibody that increases immune cells called CD56+ natural killer T cells.
Striving for tailored treatment
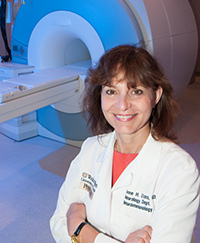
Cross notes that the alterations some of the newest MS treatments cause in the immune system could produce vulnerability to infection. She says physicians have to strike a careful balance between the benefits of new MS treatments and potential risks, some of which are not well characterized yet.
“The challenging aspect of having all these new drugs is that now we have a lot of different options to weigh,” Cross says. “We desperately need ways to determine which patients will do better on which drugs to help with these clinical decisions.”
To meet this need, Cross and her colleagues, Sheng-Kwei Song, PhD, and Dmitriy Yablonskiy, PhD, are developing new imaging techniques to better characterize what happens in the brains of MS patients before, during and after treatment.
Genetics may also provide clues. Laura Piccio, MD, Washington University neurologist at Barnes-Jewish Hospital, is working with the National MS Genetics Consortium to see whether differences in patients’ DNA can help doctors identify the best treatments for those patients.
“Many MS specialists think we now need to alter our goals for MS therapy and set our sights higher, aiming for freedom from disease activity altogether. That means no MS flare-ups, disability progression, or disease activity seen on MRI scans,” Cross says. “We cannot do that for everyone with MS just yet, but it’s becoming an increasingly feasible goal for the future.”
For more information about the MS Center and its services, please visit http://neuro.wustl.edu/research/mscenter/.






