Personalized medicine: How genetic research is transforming cancer care
By analyzing the genetic material of patients with cancer, researchers at Washington University School of Medicine are finding ways to tailor treatments
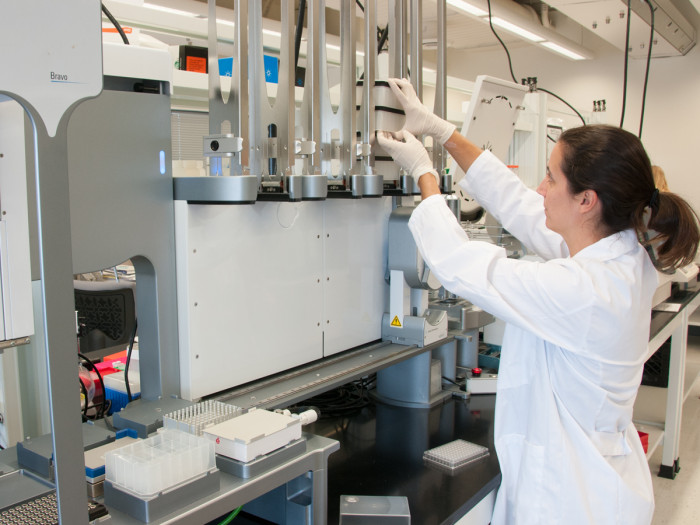
Using genomic methods, researchers are tailoring treatment for patients with cancer.
When it comes to cancer care, it is clear that a one-size-fits-all approach is not ideal. Today, armed with growing data from genetic research, physician-scientists are ushering in a new era in which cancer care is tailored to the individual. The ultimate goal: to make cancer a manageable, if not a curable, disease.
Cancer isn’t one disease; it comes in countless forms throughout the body, and no two patients are exactly alike. That poses a major challenge for physicians trying to choose the optimal treatment for each patient and for researchers working to develop better approaches to care.
For answers, physician-scientists at Washington University are turning to our genetic code. Conducting one of the world’s largest research efforts of its kind, they are gaining a more robust understanding of the roots of cancer and are applying that knowledge to tailor treatment based on the genetic signature of each patient’s tumor—an approach called personalized medicine.
“Cancer care is undergoing a great shift,” said Timothy Eberlein, MD, director of the Alvin J. Siteman Cancer Center at Barnes-Jewish Hospital and Washington University School of Medicine. “Delivering effective, tailor-made treatment to each patient based on his or her unique situation is the ultimate goal.”
Looking to our genes
Personalized medicine is based on our growing understanding of DNA, the material within all human cells that directs development and growth throughout life. Our genes are the working subunits of DNA; an organism’s entire set of genetic material is called its genome. Genomic medicine is trying to understand how genes interact with each other and the environment in ways that are relevant to health and disease.
DNA mutations, abnormalities in the genetic code that are either inherited or caused by environmental factors, can accelerate cell division and eventually lead to cancer. Scientists study the differences between DNA in normal cells and in cancer cells to identify cancer-causing mutations, learn what causes them, and determine how to stop them.
Major technological advances in recent years—many developed at the world-renowned Genome Institute at Washington University—have made genome analysis significantly faster and more economical, in turn fueling research on the genetic basis of disease.
Breaking ground
Cancer genome sequencing was pioneered by a team of researchers at The Genome Institute. In 2008, they sequenced the first-ever complete genome of a cancer patient, in an individual with acute myeloid leukemia (AML). A subsequent Washington University 2013 study, involving some 200 patients and nearly 150 researchers, revealed virtually all of the major mutations driving AML.

“We now have a genetic playbook for this type of leukemia,” says study co-leader Timothy Ley, MD, the Lewis T. and Rosalind B. Apple Professor of Oncology. “This information can help us begin to understand which patients need more aggressive treatment right up front and which can be treated effectively with standard chemotherapy.”
The field continues to mushroom, at Washington University and beyond. Genome Institute scientists, working with Siteman oncologists, have conducted similar studies for breast, ovarian, lung, uterine and other cancers. And the work is beginning to enter the clinic; Washington University’s Genomics and Pathology Services (GPS@WUSTL) now publically offers testing for 42 known cancer-related gene mutations—information physicians can use to tailor treatment, says Jon Heusel, MD, PhD, GPS@WUSTL chief medical officer and medical director of the clinical research genomic testing at The Genome Institute.
“GPS@WUSTL is bringing the promise of human genomics to the clinic,” says Karen Seibert, PhD, its director. “We use the latest gene sequencing technology and cross-reference the results to known treatment options for the patient’s particular mutations. In addition to patient care, our labs support clinical trials aimed at identifying new ways to diagnose and treat disease.”
Improving tumor classification
Ongoing research is transforming the process of defining tumor type—information key to choosing treatment. The job is traditionally done looking at tissue under a microscope; but categorizing some tumors this way is difficult, and pathologists don’t always agree. Gene testing provides a more detailed picture, allowing physicians to classify tumors based on their genetic signatures in addition to their location in the body. According to early clinical studies, the results may alter the course of treatment for some patients.
A recent study of endometrial cancer is a case in point. Clinically, endometrial cancers, found in the lining of the uterus, fall into two types, one more aggressive than the other. With a genetic analysis of tumor samples from 373 women with endometrial cancer, investigators have identified four new tumor subtypes. What’s more, one of those subtypes, identified as the less aggressive form through pathology tests alone, actually is genetically similar to the more aggressive type and requires more rigorous treatment.

“We are entering an era when tumors can be evaluated from a genomics standpoint, not just by looking at cancer cells under a microscope,” said Elaine Mardis, PhD, co-director of The Genome Institute and project co-leader. “This more comprehensive approach provides a clearer idea of the way particular endometrial cancers will behave and will be important to gynecological oncologists who treat this disease.”
Such testing has already proven its merit in breast cancer—the cancer type on the forefront of personalized medicine. In one study of 77 postmenopausal women with an advanced form of the disease, Mardis and colleagues identified distinct genetic signatures that accurately predict which patients are most likely to benefit from estrogen-lowering drugs. The drugs can reduce the size of breast tumors, enabling many women to receive breast-conserving surgery rather than a mastectomy.
“This is among the earliest cancer genomics studies to use mutations to accurately predict treatment response,” said Mardis, the lead researcher. “If our results are validated in larger studies, we think genomic information will be one more data point for physicians to consider when they select among several treatment options for their patients.”
Siteman Cancer Center coordinates patient enrollment into clinical trials, where access to experimental treatments like this is available for many cancer types. These trials are key for learning which tests and treatments are beneficial and should become mainstream care.
New applications for existing drugs
Surprisingly, some studies reveal genetic kinship among tumors in distinct sites of the body, and the implications are far-reaching. Mardis’ endometrial cancer study showed that some endometrial cancers are genetically similar to deadly subtypes of ovarian cancer and basal-like breast cancer. And in patients with breast cancer, researchers have found numerous gene changes not previously associated with breast tumors but known in patients with leukemia and prostate, colorectal, lung, skin and other cancers. Patients with these mutations may benefit from drugs already in use for those cancer types.
In another study, Washington University researchers found that some women with HER2-positive breast cancer may benefit from anti-HER2 drugs even though standard tests don’t indicate they are candidates for the drugs. The study shows the potential value of testing even a single gene of interest, said Ron Bose, MD, PhD, a Washington University medical oncologist at Barnes-Jewish Hospital.
“If we can identify mutations that we can act on, that information will help us better guide treatment,” he said. “In this case, we don’t even have to develop new drugs against HER2 mutations. It’s just a matter of finding the patients.”
Looking ahead
Gene sequencing may also help map the genetic evolution of an individual’s disease. Much like bacteria, whose habit of continually mutating can render them antibiotic resistant, tumors also constantly change, including in response to treatment. Genetic surveillance might allow physicians to monitor patients’ response to treatment and signal when it is time to try a different approach.
As research continues, cancer physician-scientists envision a brighter future.
“Already, we can treat these patients more effectively and use the word ‘cure’ more often,” said Ryan Fields, MD, a Washington University surgeon at Barnes-Jewish Hospital and a Siteman Cancer Center member. “But even if we’re not using the word ‘cure,’ we are converting cancer into a more chronic disease, so it’s more like having high blood pressure or high cholesterol—something that can be managed over time with different regimens, improving the treatment but also maximizing the patient’s quality of life.”
GENETIC SERVICES
Genomics and Pathology Services at Washington University — GPS@WUSTL
GPS@WUSTL’s Comprehensive Cancer Test evaluates 42 genes for mutations linked to
• Solid tumors: brain, breast, colon, gastrointestinal stromal, head and neck, liver and biliary structures, lung, ovary, pancreas, prostate, skin, thymic, uterus and many others
• Blood cancers: acute myelogenous leukemias, lymphocytic leukemias, lymphocytic lymphomas and others
Results can, but do not always, suggest targeted therapies based on a patient’s genes. Request service through your physician. Many insurance plans cover the cost.
Genetic counselors
At Siteman Cancer Center, patients can speak with counselors about hereditary cancer risk and genetic mutations identified through testing.
The Alvin J. Siteman Cancer Center
- The only NCI-designated comprehensive cancer center within a 240-mile radius of St. Louis
- 8,700 newly diagnosed patients annually
- 40,000 patients treated annually
- 350 member physicians and researchers
- 350 active therapeutic clinical trials
- 450 active, non-therapeutic clinical trials
Preparing for your doctor visit
The American Society of Clinical Oncology suggests that patients ask their doctors the following questions to learn more about available personalized medicine:
- What are my treatment options?
- What clinical trials are open to me?
- Are there tests available that can help guide treatment choices?
- Is this treatment considered an example of personalized medicine? If so, how?
- What are the benefits of this treatment?
- What are the potential side effects of this treatment?
- What is my chance of recovery?
Nationwide clinical trials information is at clinicaltrials.gov.
Siteman Cancer Center clinical trials information is at siteman.wustl.edu/FindProtocol.aspx.
Read more about cancer and personalized medicine at Washington University School of Medicine.
Related studies
Ley, TJ, Mardis ER, et al. DNA sequencing of a cytogenetically normal acute myeloid leukaemia (AML) genome. Nature. November 6, 2008. Read more »
Ley, TJ, Wilson RK, et al. Genomic and epigenomic landscapes of adult de novo acute myeloid leukemia. The New England Journal of Medicine. May 30, 2013. Read more »
Levine DA, Mardis ER and The Cancer Genome Atlas Research Network. Integrated genomic characterization of endometrial carcinoma. Nature. May 2, 2013. Read more »
Ellis, MJ, Ding L, Shen D, Ley TJ, Piwnica-Worms D, Stuart JM, Wilson RK, Mardis ER. Whole-genome analysis informs breast caner response to aromatase inhibition. Nature. June 10, 2012. Read more »
Bose R, Kavuri SM, Searleman AC, Shen W, Shen D, Koboldt DC, Monsey J, Goel N, Aronson AB, Li S, Ma CX, Ding L, Mardis ER, Ellis MJ. Activating HER2 mutations in HER2 gene amplification negative breast cancer. Cancer Discovery. February, 2013. Read more »






