Podcast: Racism as a public health issue
This episode of ‘Show Me the Science' focuses on racial disparities in COVID-19, as well as protests aimed at systemic racism
 Matt Miller
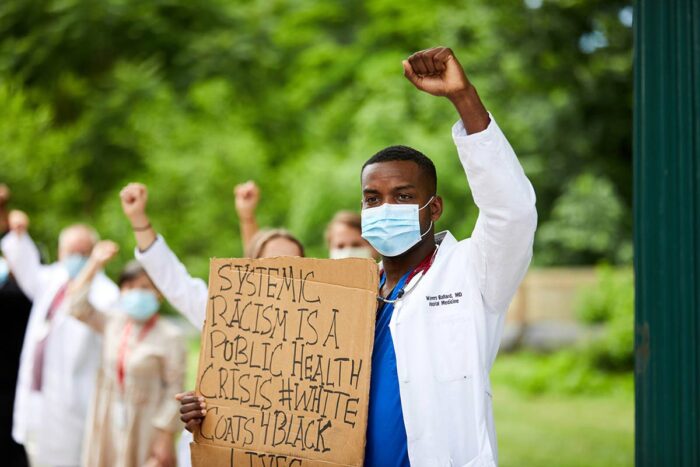
Matt MillerWenners Ballard III, MD, a hospitalist and an instructor in the Department of Medicine, took part in the White Coats for Black Lives demonstration on the Washington University Medical Campus in June. Ballard is providing for acutely ill patients who are hospitalized with COVID-19.
A new episode of our podcast, “Show Me the Science,” has been posted. At present, these podcasts are highlighting research and patient care on the Washington University Medical Campus as our scientists and clinicians confront the COVID-19 pandemic.
In St. Louis, as in much of the United States, African Americans are more likely to test positive for COVID-19. They’re also more likely to be hospitalized, to end up in intensive care and to die of the infection. Further, protests that have erupted against police violence point to another stressor shouldered primarily by African Americans.

In this episode, we discuss systemic racism — inside and outside the health-care system — and how the COVID-19 pandemic has propelled the issue to the forefront of our national consciousness. We speak with third-year medical student Kamaria Lee about her life as she studies to become a doctor during a time of massive protests and a pandemic. We also speak with Wenners Ballard III, MD. A hospitalist and an instructor in the Department of Medicine, he takes care of acutely ill patients in the hospital. These days, every one of his patients has been hospitalized for COVID-19. The majority also are people of color.
The podcast “Show Me the Science” is produced by the Office of Medical Public Affairs at Washington University School of Medicine in St. Louis.
Transcript
[music plays]
Jim Dryden (host): Hello and welcome to “Show Me the Science,” a podcast about the research, teaching and patient care, as well as the students, staff and faculty at Washington University School of Medicine in St. Louis, Missouri, the Show Me State. My name is Jim Dryden, and I’m your host this week. We’ve been focusing these podcasts on the COVID-19 pandemic and Washington University’s response. This week, we focus on race. In the St. Louis region, African Americans are four times more likely than members of other racial and ethnic groups to test positive for the coronavirus. And, as is the case in other parts of the country, they’re also more likely to be hospitalized, to be sent to an intensive care unit, and to die from the infection. But as we’ve all been reminded recently through the deaths of George Floyd, Breonna Taylor, Rayshard Brooks and others, COVID-19 isn’t the only public-health issue having an impact on people of color. We’ll speak this week about race, public health, COVID and public demonstrations with third-year medical student Kamaria Lee.
Kamaria Lee: There is this decision that people, both inside and outside the Black community, are making of what is worse: putting myself out there and potentially getting COVID, or being silent. Everybody is still afraid, especially when we have had episodes of tear gas being sprayed, and people then are coughing and tearing and rubbing their eyes. So the fear isn’t going to go away, but some people are saying, “Enough is enough,” and they’re kind of putting down their COVID fears to go out and protest.
Dryden: In fact, Washington University faculty, students and staff were recently among those at a White Coats for Black Lives event at the Washington University Medical Campus. Here’s hospitalist Wenners Ballard.
Wenners Ballard III, MD: We’re not going to stand for this. Enough is enough. And I think when you see health-care professionals, people that a lot of time you will put your life in their hands, standing up for a particular cause, it can resonate with people in a different way. And I think that touched me the most because a lot of times, you can feel like the world is against you and nobody does care. It touched people that saw the demonstration. And that’s why we did it.
Dryden: In the earliest days of the COVID-19 pandemic, as it was becoming obvious that African Americans were getting sick and dying at very high rates, medical student Kamaria Lee, who is hoping to pursue health inequities research after she graduates, wrote about the virus’s effects on the Black community, and in that essay, she said, “Each time I lose more of my people, I lose a part of me.”
Lee: There has been somewhat of a narrative in our idea that Blacks are perhaps inherently more unhealthy. But it’s a narrative that’s tied to Blacks having a higher rate of chronic conditions. It’s this idea that Blacks are more likely to have the whole list: hypertension or diabetes and things like that. And that’s really offensive when that is used as the rationale or the reason why there is a higher death rate in the Black community in St. Louis and across the country. Because a lot of that is said with this blame on the Black community, that it’s our fault that we’re just inherently unhealthy, that we could have made better choices. When really, you have to look again at history, you have to look at systemic racism and say, “What is it like to undergo racism and discrimination on a daily basis?” How is it possible for someone, whether it’s microaggressions or something more overt, to experience these things chronically throughout their life and have it not affect their health? It does. It affects your health. It has this extra load on your body. And all of that affects baseline level of health, and then it also can be amplified as we’re seeing in a pandemic or with many other illnesses.
Dryden: And I want to know how that’s affected you as you are pursuing your training.
Lee: Being a medical student and knowing that the data is out there, that Blacks have a higher death rate, are more likely to be hospitalized and infected with COVID-19, and also already having experienced what it’s like to be a Black medical student. There aren’t many Black students in higher education in general, and that’s true in medical training as well. So already having experienced, what it feels like a special bond with the Black patients that I’ve interacted with in the hospital due to a cultural congruence, perhaps in some cases, but not all, increased trust. And then hearing about this public health crisis, or rather living through this public health crisis, knowing that it’s those patients or patients who look like me who I’ve already related to on a very deep level in the hospital that are some of those that are most affected. Even just the anxiety and the mental-health aspect of knowing that your community is being more affected is also something that they’re going through and a struggle that we share.
Dryden: And you wrote you’ve seen extra fear in your people’s eyes when they’re in the hospital and there are few, if any, clinicians who look like them. So you also say that you felt distrust even of you sometimes because, for some, that white coat makes you a part of the ivory tower. I want to know, can you talk a little bit more about that?
Lee: Yeah. I think it’s important to always know the historical context in which we’re working. Even for myself being a part of the community, educating myself on what happened before I was here. And so just looking back, we have, from the 1930s to the 1970s, the Tuskegee syphilis study, in which Black men were experimented on in order to see what would happen with untreated syphilis. So during that time, penicillin was seen to be a cure for syphilis, but the men were not told about that, and their syphilis continued to be untreated, which is completely unethical and horrifying. There are also instances of Black bodies being robbed from graves to be used during medical dissections historically. And so not everyone in the Black community knows all of this historical detail. Some do, but some of that history is a part of the distrust. Or even more recently, segregation hospitals or knowing that your life isn’t seen as the same when you walk into the health-care system because you were taken to a different hospital and some clinicians wouldn’t allow you into their clinic. So all of that has created a long history and a reasonable history of distrust of, yeah, white clinicians, non-Black clinicians, but also the system. And a part of me being a clinician means that my identity is multiple things. I’m a Black woman, but I’m also part of the health-care system. And so sometimes skin color or even the same culture, a similar background, isn’t enough to kind of negate the distrust that, like I said, is rightfully there for many reasons.
Dryden: Is this a good time to be a medical student? I mean, obviously the pandemic affects the rotations that you can do, your interaction with patients. On the other hand, this is a once-in-a-century sort of public-health crisis combined now with a public-health crisis that’s been going on in the United States for at least 400 years.
Lee: Going to medical school now with the COVID-19 pandemic and with the current changes that we’re seeing, more people in society want to make towards– or against racism. I think a lot of people in the Black community and other minority communities have been pushing for people to realize how bad racism is, which sounds silly because it’s been going on for decades and hundreds of years. But I feel like there has been this hope for others and enough of other people to finally be fired up to make change. And I think that while it’s not changing everyone’s minds and some people are more cynical about how much change can actually be made, I think it’s a critical moment for people in medical school to understand that you need to acknowledge racism and be actively working against racism in order to be an adequate clinician.
Dryden: When you finish medical school, somebody’s going to make a speech and say to you and your classmates that you’re part of the future, you will write the future. But you wrote in your essay that it’s hard not to be intimidated by the enormity of the problem here. So how can you and your classmates make that future different and better?
Lee: One thing I recently encouraged my classmates to do is to all put health inequity research as something that they do. Or if they’re interested in research, health equity advocacy is something that they do. I have a bachelor’s in sociology from college. And like I said, right now and in the future, I hope to continue health inequities research. And while it’s great that I can define myself that way and say, “This is who I want to be in my academic career,” it’s actually sad that I can define myself that way because it should just be something that all clinicians are doing. It shouldn’t be a distinguishing factor. It should be, “I’m in the medical field. I’ve taken an oath. And I’m here to fight against inequities, fighting against racism’s effects on health.” And so that’s something that I really hope my classmates will all do, is define themselves the same way I have defined myself so that it’s not actually a unique way to go about their careers.
Dryden: Several WashU physicians, others recently, that participated in the White Coats for Black Lives. What message was sent that day, and does it relate in any way to the inequities that you see regarding COVID-19?
Lee: I think it represents an intent, it represents an action. But as far as how large the issue is of racism and how significant racism is as a threat to public health, as we’ve seen with the police brutality or just several unjust murders, it’s a very small step. It is up to everyone, regardless of their race or ethnicity or their own background or privilege, to walk in what they did at the protests every single day. To be more cognizant of how they are treating their patients, to understand, “Maybe if I’m not from the same culture, that doesn’t mean there is no chance of relating,” and so to at least try. There is a lot of things that need to happen in the micro-level within each patient interaction, with interactions of all of their trainees, as well as in their own personal lives and how they raise their children. And so something that’s a powerful image can represent intent and hopefully represents a promise. But it’s a very small step in what actually needs to be done both by individuals and at institutional levels. But some people are saying, “Enough is enough” and are kind of putting down their COVID fears to go out and protest.
Dryden: One of those young African Americans wearing a white coat was Wenners Ballard III. He’s a hospitalist at Washington University and Barnes-Jewish Hospital in St. Louis. That means he takes care of acutely ill patients in the hospital. And for the last several weeks, that has meant patients who have COVID-19.
Ballard: Ever since this really ramped up in about late February or early March, Barnes dedicated a certain group of physicians to only taking care of COVID patients to sort of limit the exposure to a lot of physicians. And I was one of those.
Dryden: Is that a scary thing from your perspective, or does it mean that there are certain folks in your life that you can’t see because you’re taking care of these patients?
Ballard: I don’t know if I would call it scary. It’s definitely in the back of your head where you do hear of younger people catching this and having poor outcomes. But it’s definitely a lower mortality rate in people in my demographic age group-wise. But it is still worrisome. And I wasn’t able to – my dad has multiple myeloma and he’s currently on chemotherapy, so I wasn’t able to go back and see him, where I probably otherwise would have. So in that way, it did affect me. But you kind of put all that to the side when you see how many people are affected and kind of need your help. It just feels like your calling and this is what you did all this for in the first place. So you kind of step up to the plate and don’t really think about the other things.
Dryden: African Americans have been hit harder than many other communities. Is that what you’ve experienced on the floors at Barnes-Jewish?
Ballard: Absolutely. Definitely, African Americans have been hit disproportionately by COVID, especially in St. Louis. I think when you look at the statistics across the nation, what you’re seeing is African Americans being disproportionately affected, but specifically African Americans that live in certain parts of the country. So for instance, if you look at New York, which is kind of the epicenter for all of this, people that lived in certain counties in New York City had a threefold higher rate of infection and a sixfold higher rate of dying. If you look in cities like Chicago that’s much closer, the infection rate among African Americans, I believe, was around 50% –
Dryden: Meaning that 50% of the COVID cases in Chicago involved African Americans.
Ballard: And the mortality rate among African Americans was around 70%, but they only make up 30% of the population in Chicago. It’s mostly centered around on the south side of Chicago. So it has a lot to do with socioeconomic status.
Dryden: These racial disparities are not unique to COVID-19, correct?
Ballard: They are not. And I think it’s interesting – I was actually thinking about this the other day – I think COVID-19 kind of pulled back the shade a little bit and showed us like, “Wow, these health disparities are real, and there’s something that really needs to be done about it.” Sort of like how when everybody saw that video of the knee on his neck, people said, “Wow, enough is enough. There’s something that we need to do about it.” And you’re seeing some change occur already. I hope that same thing will happen in the health-care community and we start to do more things to try to bridge the gap. When you aren’t able to do social distancing because you work at the local grocery store, you work at the gas station, you work at places where you’re not able to work from home, you’re not able to telework, you’re not really able to social distance. And also, when you live in these areas, the household density is higher, meaning there’s a lot more people under one roof. And I think St. Louis is a prime example, when you look at the “Delmar Divide,” we’ve known about these health-care disparities for a very long time. I had a lady that was 50 years old. She had no medical co-morbidities. And she could not stop going to work because if she did, her lights would be cut off, her water’s going to get cut off. She got COVID. She ended up on the highest form of life support we had called ECMO. Ultimately, she did walk out of the hospital. And she is one of the very rare cases that we see. And she almost didn’t make it. And it’s just very shocking to see a 50-year-old that’s otherwise very healthy that probably could have avoided this if she could have teleworked, if she had been able to not worry about her lights, if she had, you know, a lot of things.
Dryden: What can medical professionals and the health-care community in general do about this at the moment? Well, you know, on the George Floyd issue, we can say, “Well, let’s take some steps to monitor police in different ways.” On the health-care front, what can someone like you do?
Ballard: It’s complicated, and it’s going to take a lot and a long time, but I think what we can start doing right now is working on our own implicit biases, kind of addressing how we look at each individual patient. So I know a lot of times colleagues of mine walk into a room and see a particular patient and adjust the way they speak to them or adjust their expectations of how that interaction is going to go. I think sometimes people – and I don’t think people do it maliciously, honestly. I think it’s just because of lack of knowledge and lack of exposure. I don’t think people should be ashamed to say that they don’t really know how to go about these interactions or how to make sure somebody is understanding what they’re saying. Educating our patients more is a big part of this. That’s something that we can do every day when we walk into a patient’s room. And I think doing our best to check our biases at the door is another big thing that we can do right now. I mean, it’s something that we definitely need to start doing, but we also need to work on a bigger change in the country overall.
Dryden: You recently attended the White Coats for Black Lives event. What motivated you to do that? And what message were you, and the other physicians and health-care workers participating trying to send?
Ballard: I think the message that we’re trying to send is, overall, one, solidarity and unity and standing up for what’s right and showing the people in this country and the rest of the world that we’re not going to stand for this, enough is enough. And I think when you see health-care professionals, people that a lot of times you will put your life in their hands, standing up for a particular cause, it can resonate with people in a different way. And I think, when I saw a lot of the people driving by, it was very interesting to see the varying reactions. There were some people in tears just being so touched by it, some people honking their horns, clapping, cheering. Some people scowling. Some people yelled out some things as they drove by. What I saw overall was overwhelming support. And I think that touched me the most. Because a lot of times you can feel like the world is against you and nobody does care, but to see that amount of people in that position caring that much, that they walk out of their jobs, they stand on the street, they hold up signs, they kneel for 8 minutes and 46 seconds, to see that many people doing that in that profession, it touched me. So I know that it touched people that saw the demonstration. And that’s why we did it. We did it to show that this can’t keep happening and it’s not going to keep happening and we’re going to do something about it.
Dryden: People were wearing masks. They were socially distancing. When you see some of the other protests where maybe masks aren’t as ubiquitous and where maybe people either by choice or because they’ve sort of been corralled by police are very close together, does that worry you as the guy that might be treating some of these folks?
Ballard: Absolutely. Absolutely. Because of course, a lot of the people at these protests are 50 and younger. You would probably be asymptomatic if you’ve got it, honestly, or have mild symptomatology from it, but you could pass it on to somebody that’s not. So I think it is important that people do, especially for the time being, keep their masks on. Especially at these protests, we get really excited, we’re loud, I think it is important to try to social distance as best you can and wear a mask. And if you do that, then don’t let it deter you, and get out there. Get your message across. That’s also important because they’re both health-care crises.
[music plays]
Dryden: Ballard and Lee say many things must change to address the health-care disparities that put people of color at greater risk for COVID-19 and other illnesses. And both say they’re committed to becoming part of the solution and encouraging their colleagues in medicine to do the same.
Show Me the Science is a production of the Office of Medical Public Affairs at Washington University School of Medicine in St. Louis. The goal of this project is to keep you informed and maybe teach you some things that will give you hope. Thanks for tuning in. I’m Jim Dryden. Stay safe.






