Potential new target identified for treating itch
Findings suggest nerve receptors work in concert to transmit itch signals
 Robert Boston
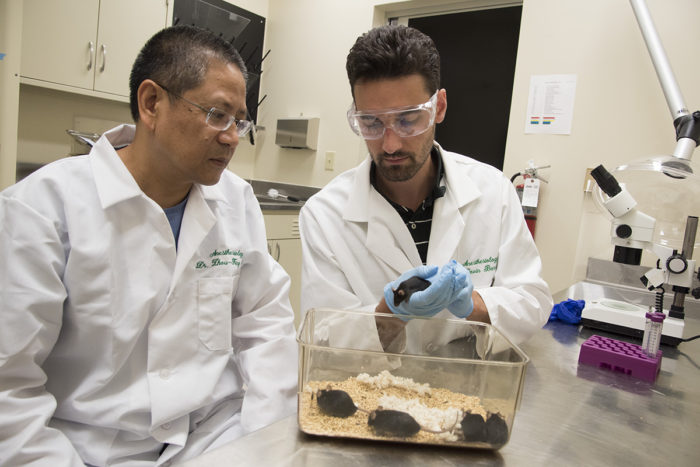
Robert BostonZhou-Feng Chen, PhD (left), director of the Center for the Study of Itch at Washington University School of Medicine in St. Louis, and postdoctoral research scholar Devin M. Barry, PhD, have found that certain pathways in the sensory neurons of mice can work together to transmit itch signals. The discovery may help scientists find more effective ways to make itching stop.

Researchers have found how sensory nerve cells work together to transmit itch signals from the skin to the spinal cord, where neurons then carry those signals to the brain. Their discovery may help scientists find more effective ways to make itching stop.
The researchers, at Washington University School of Medicine in St. Louis, report the new findings online July 19 in the journal Science Signaling.
“By interfering with the activity of sensory neurons, we may be able to inhibit multiple types of itching,” said principal investigator Zhou-Feng Chen, PhD, director of the university’s Center for the Study of Itch. “It appears there is cross-talk between pathways called calcium channels in sensory nerve cells that process the itch signal.”
The researchers studied calcium channels in neurons, which allow for the transport of calcium ions from one nerve cell to another, helping the cells transmit itch signals from the skin to other cells in the spinal cord.
Chen’s team focused on the dorsal root ganglion of laboratory mice, a structure near the spinal cord that is full of sensory nerve cells. It processes signals from the skin and transmits them to neurons in the spinal cord.
The researchers looked at on how neurons in the dorsal root ganglion process and transmit two types of itch signals. One signal, called histamine-induced itching, is caused by bug bites, for example, and responds to antihistamine drugs, such as Benadryl.
The other type of itching, called called chloroquine-induced itching, often is experienced by malaria patients who take the drug chloroquine to control their symptoms.
Scientists had thought that histamine signals traveled through one type of calcium channel, while chloroquine signals traveled through a different channel.
But when scientists genetically engineered mice without the channel that processes histamine signals and then exposed the animals to histamine, the mice still scratched. The mice also scratched if they lacked the calcium channel that transmits chloroquine-induced itch signals and were exposed to chloroquine.
Chen’s team — puzzled by such results — spent years looking for an explanation. After dozens of experiments, the scientists found that a third calcium channel called TRPV4 can transmit both types of itch. And they also learned that TRPV1, the channel that transmits histamine-induced itch, also plays a role in chloroquine-induced itch by helping TRPV4 process itch signals. The fact that it is involved in both of those types of itch raises the possibility that the TRPV4 channel also plays a role in other types of itching, including chronic itch.
“The big surprise is that although these different types of itching have different causes, these two channels in sensory cells can work together to signal both types of itching,” said Chen, a professor of anesthesiology, of psychiatry and of developmental biology. “We found that the TRPV1 channel that processes histamine-induced itch seems to work as a kind of molecular chaperone in the sensory neurons, helping the other channels process itch signals and transmit them to the spinal cord.”
Chen said proving that the channels work in concert helps explain how sensory cells can process numerous types of environmental signals, including itching that results from different things. It also suggests the channels his team identified may be targets for treating itch.
“It gives us new therapeutic targets upstream of the neurons in the spinal cord,” he explained. “By targeting a single channel in the periphery, it may be possible to reduce histamine-induced itching, chloroquine-induced itching and even types of chronic itching that don’t respond to current therapies.”






