Research sheds light on asthma and respiratory viruses
Washington University researchers are studying respiratory viruses to better understand how they contribute to asthma and other conditions
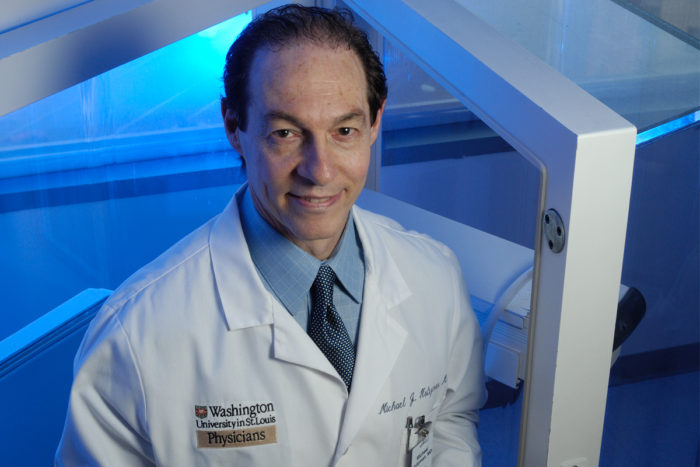
Michael Holtzman, MD, and his colleagues are studying why patients with asthma have more difficulty with respiratory viruses than people without asthma.
People with asthma often have difficulty dealing with respiratory viruses such as flu, the common cold, and more recently enteroviruses, and researchers have struggled to explain why.
There is debate among asthma researchers over why patients with asthma might have more trouble dealing with respiratory viruses than people without this common breathing disorder. The controversy has centered on the role of interferon proteins that are crucial for defense against viruses.
Interfering interferon?
Pulmonologist Michael Holtzman, MD, and his colleagues looked at two common airway viruses—influenza A virus and respiratory syncytial virus (RSV)—and the interferon response that they triggered in airway cells sampled from 11 patients with mild to severe asthma and seven control subjects without asthma.
“One school of thought says there is a defect in interferon production—that patients with asthma don’t produce enough interferon,” said Holtzman. “But we couldn’t find any significant differences between the two groups. In fact, we were struck by how similar they were.”
To find out whether interferon might be less effective in patients with asthma, the investigators compared the downstream activation of genes by interferon and found it to be remarkably similar in both groups of patients. They also measured similar amounts of virus living in the cells at various points of time during the study, indicating that the immune system’s battles against the viruses progressed similarly in both groups.
“Whatever is causing asthmatics and non-asthmatics to experience differences in how well they recover from these respiratory infections—why patients with asthma are more likely to end up in the hospital, for example—this interferon mechanism is not the deciding factor, based on what we’ve seen so far,” Holtzman said.
Next up: Enterovirus
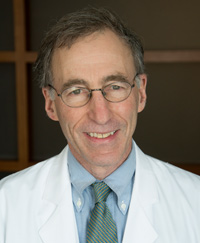
Researchers are also studying the genomics of enterovirus, which has caused severe illness nationwide. Infectious disease specialist Gregory Storch, MD, and his colleagues sequenced one nearly-full and eight partial enterovirus D68 strains from children at St. Louis Children’s Hospital. The sequences were all very similar to one another but differed slightly from published genomes of other Midwestern strains. The work is expected to be helpful in designing better diagnostic tests and in helping understand the ways in which the virus spreads and makes people sick.
Holtzman and his colleagues are also working with the enterovirus samples to isolate the virus and determine whether it triggers a different type of immune response in people with and without asthma.
Like the common cold virus and some other respiratory viruses, enterovirus depends on a viral protease enzyme to assemble itself in the host cell. Holtzman and his colleagues have already worked out how the immune system destroys this viral protease and thereby blocks viral assembly. Next, they plan to see whether people with asthma may have differing abilities to attack the viral protease and control the viral infection.
In concert with this approach, Holzman and his colleagues are also designing compounds that can block this system for viral assembly and provide a new form of treatment for these types of respiratory infections. They are in the process of obtaining approval for a clinical trial of one of their first formulations of an antiviral drug.






