Study finds marker of aggressive prostate cancer
May inform future tests to help doctors decide how best to treat prostate tumors
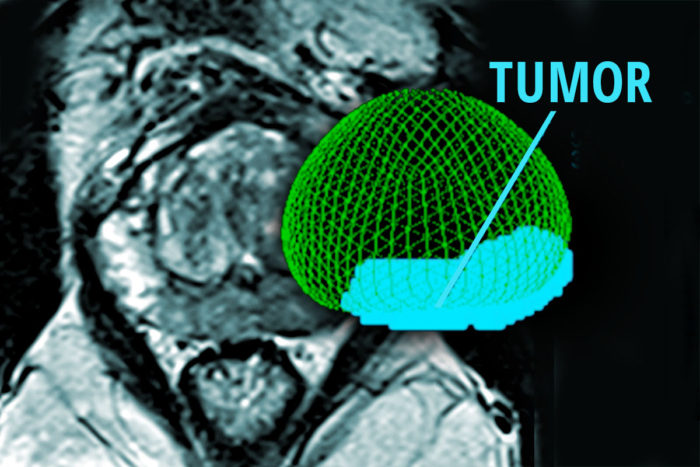 Kathryn Fowler/Eric Young
Kathryn Fowler/Eric YoungStudying prostate tumors, researchers have identified a marker of aggressive prostate cancer. The findings could guide the design of future clinical tests to help doctors determine whether a patient has slow-growing or aggressive cancer. Shown is a scan of a patient with prostate cancer and (in color) a 3-D rendering of the prostate and tumor.
The level of a specific molecule present in prostate tumors is an indicator of whether the cancer is aggressive and likely to spread, according to new research from Washington University School of Medicine in St. Louis.
The study, available online in the journal European Urology, may inform future clinical tests that help doctors decide how best to treat prostate tumors. Many men with prostate cancer have slow-growing tumors that do not require surgery, radiation or other treatments that can leave patients impotent, incontinent or both. But doctors often have difficulty telling the difference between these indolent tumors and those that will prove to be more aggressive.
“Distinguishing patients who have indolent versus aggressive prostate cancer is probably one of the biggest challenges in the field,” said senior author Christopher A. Maher, PhD, an assistant professor of medicine. “Our study suggests that levels of a molecule called PCAT-14 may be a marker of whether the tumor is likely to be aggressive, helping doctors decide whether to intensify a patient’s treatment.”
The scientists measured levels of PCAT-14 from prostate tumors after their surgical removal. Maher said one of his group’s goals is to design a noninvasive method, such as a urine test, to make the same measurement.
The scientists found that levels of PCAT-14 — an RNA molecule — were elevated across 180 prostate cancer patients treated at three different institutions. Analyzing another 910 tumor samples from patients with known treatment outcomes, the researchers also showed that the patients with more aggressive tumors, perhaps surprisingly, had lower levels of PCAT-14. Patients with slow-growing tumors had higher levels of the molecule. That may seem counterintuitive, but according to Maher, the data suggest that high levels of this RNA molecule suppress tumor spreading. So when levels decrease, that suppression is lost and the cancer cells are free to metastasize.
Past work by Maher and his colleagues has identified PCAT-14 as one of 121 similar RNA molecules strongly associated with prostate cancer. Many of the other PCAT molecules they found associated with a variety of cancers, including prostate, but PCAT-14 was specifically found only in prostate cancer. RNA is similar in structure to DNA and serves various functions in cells, especially in turning genes on and off.
“We looked at all similar RNA molecules in these prostate tumors,” Maher said. “Only PCAT-14 was consistently altered in all prostate cancer patients and able to distinguish indolent and aggressive disease.”
Working with aggressive prostate cancer cells in the lab, the researchers showed that dialing up levels of PCAT-14 appeared to build up barriers to cancer spreading, slowing the growth and mobility of these normally aggressive cells. Likewise, dialing down levels of PCAT-14 appeared to remove barriers to spreading, making these cells even more aggressive, increasing the number of cells and their ability to move.
Maher and his colleagues also showed that low levels of PCAT-14 were associated with poor response to androgen deprivation therapy, a hormone-based treatment for prostate cancer that is less toxic than chemotherapy and radiation therapy. Prostate tumor growth often is driven by male hormones, such as testosterone. Depriving prostate tumors of hormonal fuel can slow or stop growth, but some tumors grow even in a state of hormone deprivation.
“We suspect that PCAT-14 may be a good predictor of whether patients will respond well to androgen deprivation therapy,” Maher said. “Low PCAT-14 means the cells are likely to grow and spread even when deprived of androgens.”
With improving diagnosis and treatment in mind, Maher said the development of a noninvasive test to measure levels of PCAT-14 could reduce the need for biopsy or removal of the prostate. This is an advantage of identifying a molecule that is only present in the prostate, according to Maher. In theory, if this molecule can be detected in a urine sample, for example, there would be no question it would indicate a problem with the prostate rather than some other organ, such as the kidney or bladder.






