Study prompts new ideas on cancers’ origins
Mouse study shows mature cells can create precancerous lesions
 Matt Miller
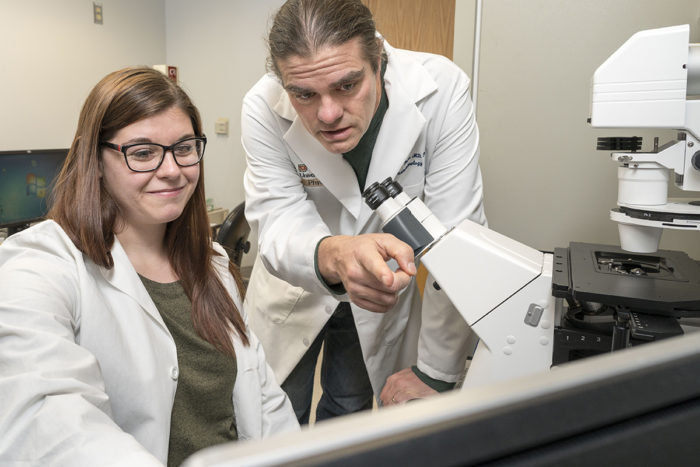
Matt MillerGraduate student Megan Radyk and Jason Mills, MD, PhD, led a study revealing that although many cancer therapies target rapidly dividing stem cells, mature cells also seem to play a key role in initiating cancer, at least in forming precancerous lesions.

Rapidly dividing, yet aberrant stem cells are a major source of cancer. But a new study suggests that mature cells also play a key role in initiating cancer — a finding that could upend the way scientists think about the origins of the disease.
Researchers at Washington University School of Medicine in St. Louis have found that mature cells have the ability to revert back to behaving more like rapidly dividing stem cells. However, when old cells return to a stem cell-like status, they can carry with them all of the mutations that have accumulated to date, predisposing some of those cells to developing into precancerous lesions.
The new study is published online in the journal Gastroenterology.
“As scientists, we have focused a good deal of attention on understanding the role of stem cells in the development of cancers, but there hasn’t been a focus on mature cells,” said senior investigator Jason C. Mills, MD, PhD, a professor of medicine in the Division of Gastroenterology. “But it appears when mature cells return back into a rapidly dividing stem cell state, this creates problems that can lead to cancer.”
The findings, in mice and in human stomach cells, also raise questions about how cancer cells may evade treatment.
Most cancer therapies are aimed at halting cancer growth by stopping cells from rapidly dividing. Such treatments typically attack stem cells but would not necessarily prevent mature cells from reverting to stem cell-like status.
“Cancer therapies target stem cells because they divide a lot, but if mature cells are being recruited to treat injuries, then those therapies won’t touch the real problem,” said first author Megan Radyk, a graduate student in Mills’ laboratory. “If cancer recurs, it may be because the therapy didn’t hit key mature cells that take on stem cell-like behavior. That can lead to the development of precancerous lesions and, potentially, cancer.”
Studying mice with injuries to the lining of the stomach, the researchers blocked the animals’ ability to call on stem cells for help in the stomach. They focused on the stomach both because Mills is co-director of Washington University’s NIH-supported Digestive Disease Center and because the anatomy in the stomach makes it easier to distinguish stem cells from mature cells that perform specific tasks. Even without stem cells, the mice developed a precancerous condition because mature stomach cells reverted back to a stem cell state to heal the injury.
Analyzing tissue specimens from 10 people with stomach cancer, the researchers found evidence that those same mature cells in the stomach also had reverted to a stem cell-like state and had begun to change and divide rapidly.
The Mills lab is working now to identify drugs that may block the precancerous condition by preventing mature cells from proliferating and dividing.
“Knowing these cells are leading to increased cancer risk may allow us to find drugs to keep mature cells from starting to divide and multiply,” Mills said. “That may be important in preventing cancer not only in the stomach and GI tract but throughout the body.”






