Taylor Family Institute targets psychiatric illness research
Washington University has received $20 million to fund the Taylor Family Institute that will help develop new therapies for psychiatric disorders
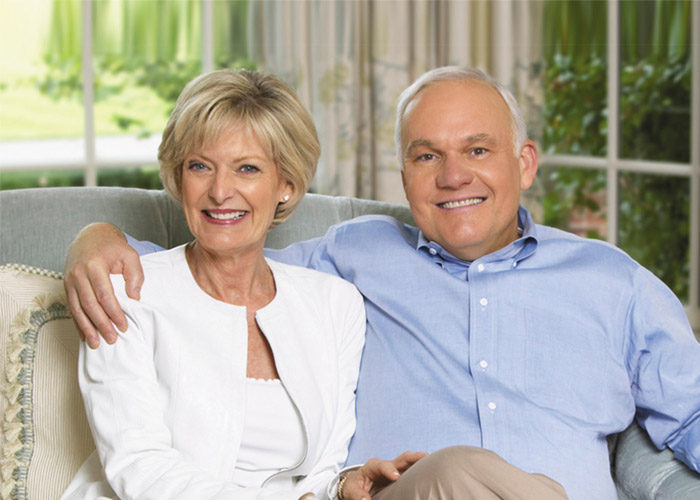
Barbara and Andrew Taylor committed $20 million to fund the Taylor Family Institute for Innovative Psychiatric Research.
Up to 30 percent of adults in the United States suffer from a psychiatric illness at some point in their lives, and those illnesses account for more than 40 percent of all disabilities.
Modern neuroscience and genetics are providing new insights into the underlying mechanisms that contribute to psychiatric illnesses. But despite that progress, relatively few new and more effective treatments have come to market.
In fact, the last class of psychiatric drugs developed successfully were selective serotonin reuptake inhibitors (SSRIs), for treating depression, and new-generation antipsychotic medications for illnesses such as schizophrenia. Although those drugs tend to be more effective than older medications, they target the same systems in the brain as did psychiatric drugs that were available in the 1950s and 1960s.
Now, with the support of a major gift from Andy and Barbara Taylor and the Crawford Taylor Foundation, Washington University researchers at Barnes-Jewish Hospital are continuing to advance the science underlying the diagnosis and treatment of psychiatric illnesses.
The Taylors committed $20 million to the Department of Psychiatry at Washington University School of Medicine to fund the Taylor Family Institute for Innovative Psychiatric Research, a center focused on developing new and more effective therapies for psychiatric disorders.
Focus on neurosteroids
The Taylor Family Institute involves laboratory and clinical research collaborations among faculty in several Washington University departments, including psychiatry, anesthesiology, developmental biology, radiology, neurology and internal medicine.
Scientists at the institute initially are focusing their attention on neurosteroids—chemicals that occur naturally in the brain that are involved in brain networks used for cognition, emotion and motivation. Disruptions in neurosteroid levels can contribute to mood disorders such as depression, anxiety disorders, schizophrenia, alcoholism, sleep disorders, chronic pain, epilepsy, and neurodegenerative illnesses such as Alzheimer’s disease.
Members of the institute have been conducting research on natural and synthetic neurosteroid molecules for several years, investigating their use as potential anesthetic agents as well as treatments for psychiatric illnesses.
Current evidence suggests that the production of neurosteroids in the brain is affected by stress and by particular disorders such as depression, so institute scientists believe that replacing or enhancing these depleted steroids may be effective in alleviating that stress response in order to make the brain function more normally.
The institute’s first director is Charles Zorumski, MD, the Samuel B. Guze Professor of Psychiatry and Neurobiology and head of psychiatry at Washington University and Barnes-Jewish Hospital.
“We believe the Taylors’ gift will allow us to do incredible things for the field of psychiatry,” he says. “We want to push the development of new therapies involving neurosteroids to benefit patients who continue to struggle with psychiatric illness, and we believe that these resources, backing our existing scientific and clinical expertise, could quickly lead to new and better treatments.“
Clinical trial partnership

Zorumski and other members of the institute are collaborating with Sage Therapeutics, a neuroscience-product-focused company creating novel medicines to treat important central nervous system disorders, to get new neurosteroid drugs into clinical trials as quickly as possible. Those clinical trials won’t occur in St. Louis to avoid any conflicts of interest because Zorumski and some other members of the institute also serve as scientific advisors to Sage. The goal of the collaboration is to significantly cut the lag time between laboratory discoveries and studies involving human patients.
In fact, Sage recently announced the first use of a neuroactive steroid to treat a patient for severe seizures.
“That case-study worked out very well, which is a big deal for moving neurosteroids forward as potential therapeutic agents,” Zorumski says. “That could open the door for the testing of other neurosteroids in future human trials.”
One potential agent that’s being developed involves a class of chemical messengers that are related to cholesterol, the fat in the bloodstream that can cling to artery walls and contribute to cardiovascular disease. Called oxysterols, these agents are being investigated for their potential to enhance cognitive function or for use as antipsychotic drugs.
To read and hear more about the institute, visit the Taylor Family Institute for Innovative Psychiatric Research.
Note: Charles Zorumski, MD, is a scientific advisor for Sage Therapeutics.






