Washington People: Patrick Jay
Pediatric cardiologist seeks keys to preventing congenital heart defects
 Karen Elshout
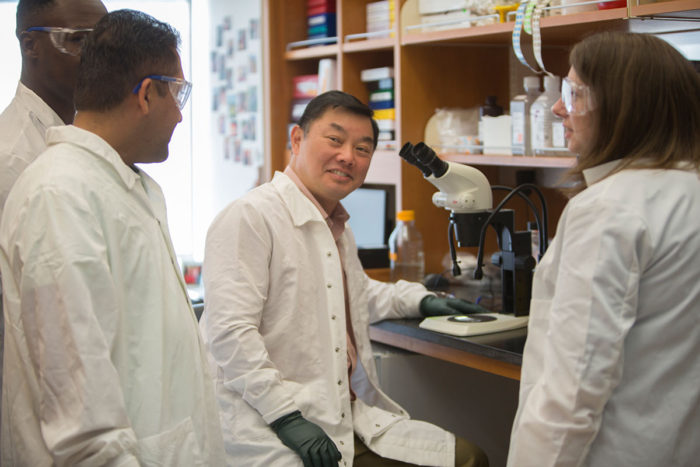
Karen ElshoutPatrick Jay, MD, PhD, (center) is a pediatric cardiologist studying the genetic and environmental roots of congenital heart defects. Members of his lab include (from left) Ehiole O. Akhirome, an MD/PhD student; Suk D. Regmi, a senior research technician; and Julie M. Nogee, MD, a clinical fellow in newborn medicine.
As a medical student, Patrick Jay took an interest in pediatrics because the discipline seemed to him like a monumental lesson in genetics. Every young patient who came to the hospital — almost regardless of the reason — indicated something interesting about basic human biology.
“Thousands of kids in St. Louis may be exposed to the same virus, for example, but only a few get sick enough to be hospitalized,” said Jay, MD, PhD, an associate professor of pediatrics. “What’s different about them? Unlike adults, children’s diseases are much less influenced by lifestyle. Pediatric diseases tell you something fundamental about human biology.”
Jay’s decision to focus on cardiology came from a more practical place. He felt that his most talented peers were going into cancer research and decided he had a better shot at making an impact in cardiology, where he thought the competition to make new discoveries would be less intense.
“I was definitely wrong about that!” he said.
In his focus on cardiology, Jay considers himself fortunate in timing, both personally and professionally — personally, because he met his wife, Kathleen Jay, on the cardiology service during his fellowship at Boston Children’s Hospital. She was an electrophysiology nurse practitioner caring for patients with pacemakers, and he remembers offering to carry the heavy equipment she needed to lug around the hospital.
Professionally, Jay’s timing was fortunate in that he was offered an opportunity to work in the lab that had discovered the first gene regulating heart development in mice. Complete loss of this gene, called NKX2-5, in mice causes heart development to stop early. The equivalent gene in fruit flies is dubbed tinman after the character in “The Wizard of Oz.” A fly missing this gene, like the Tin Man, has no heart.
Mutations in NKX2-5 had been found in families with histories of congenital heart defects, such as holes in the heart’s chambers or problems with the heart’s electrical signals. In infants and young children, some with only one working copy of the gene had severe heart defects. But others with the same genetic problem had normal hearts. Jay wondered what was different about these groups of children with the same genetic mutation that led to severe heart defects in some but not others. Sensing a clue to human biology, Jay began to study mice with the same genetic mutations.
Early studies did not seem promising at first. Mice with one working copy of the gene had some problems but nothing approaching what was seen in people with equivalent genetics.
“Back when I had a lot more time on my hands, I would do an autopsy on every mouse,” Jay said. “And one day I discovered a ventricular septal defect — a hole between the lower chambers of the heart — in an adult mouse with an unusually large heart. It was a rare find, and a light bulb went off. In retrospect, it’s obvious, but mouse research on congenital heart disease had run into a block because we were studying adult mice. If you want to see heart defects in mice, you have to study the newborns. The mice we needed to study don’t survive to adulthood.”
Still, a seemingly simple decision to study mouse pups did not solve the problem. Jay realized the pups with severe congenital heart defects were not only dead — they didn’t even seem to exist. Mouse mothers, likely in an effort to better care for their healthy young, often eat dead or dying pups.
“About 15 percent of the mice with the genetic mutation were missing when the mice were big enough to be weaned from their mothers. They were lost as newborns, at the equivalent time that babies with heart defects come to medical attention,” he said. “As I was starting my own lab, we learned that if we want to find pups with heart defects, we have to identify them soon after birth. The most severe heart defects will cause death around six hours of age and moderately severe defects by two days.”
So Jay instituted what is basically a system of doing rounds on his mice, as doctors do rounds in hospitals to check on their patients.
 Karen Elshout
Karen Elshout“When I started this project years ago, I did a back-of-the-envelope calculation,” he said. “I decided I would drop the project if I did not find a mouse with a serious heart defect among the first 60 hearts examined. Fortunately, mouse No. 60 had a defect. An awesome team of students has since gone on to examine the hearts of 20,000 or so pups. They have made some unique and incredible discoveries.”
Jay’s work has deepened knowledge of the origin of heart defects, but he considers his family his most important achievement. When he is not in the lab or seeing patients, he serves as the scoutmaster for his sons’ Boy Scout troop, which some who know him find surprising.
“I’m not an outdoors guy,” he said with a laugh. “I have limited outdoors and knot-tying skills, so on a recent campout, I taught the scouts the concept of doing hospital rounds. I go with what I know.”
And what Jay knows, or has learned over many years of research, is that the genetic mutation that leads to congenital heart defects is impacted by multiple factors — interactions with other genes and environmental cues — that determine whether the mouse pup, or child, will actually have a heart defect.
“In many ways, we’re asking the opposite of a typical research question,” said Jay, who treats patients at St. Louis Children’s Hospital. “Instead of studying the abnormal and asking, ‘Why is this abnormal?’ we’re studying a genetic mutation that should cause a problem but often doesn’t. We’re asking, ‘Why is this individual normal?’ If we can understand how a normal heart develops even in the presence of a disease-causing mutation, perhaps we can give what that person has to everyone else as a means of prevention.”
Jay said that today, treatments for heart defects are approached much like plumbing problems: Patch the hole, bypass the block. He hopes to one day see more of a preventive approach that helps ensure that the pipes and electrical circuits of the heart are laid down properly to begin with, during the earliest stages of development.
With that in mind, Jay and his colleagues published a study in Nature in 2015 showing that through exercise, older mouse mothers with the genetic mutation could reduce their risk of bearing pups with heart defects.
“This is a complex problem,” Jay said. “We’re still unraveling the details of how environment and genetics interact to cause severe defects, mild defects or none at all. There appear to be critical genetic interactions. If we could target them, we might be able to prescribe a pill or exercise to mothers to help prevent heart defects in their babies, just as we now prescribe folic acid to prevent neural tube defects.”
 Courtesy of Patrick Jay
Courtesy of Patrick Jay





