WashU Medicine leads 2 major pandemic preparedness research projects
Two grants totaling $30 million a year for 3 years support efforts to design vaccines, drugs for understudied virus families
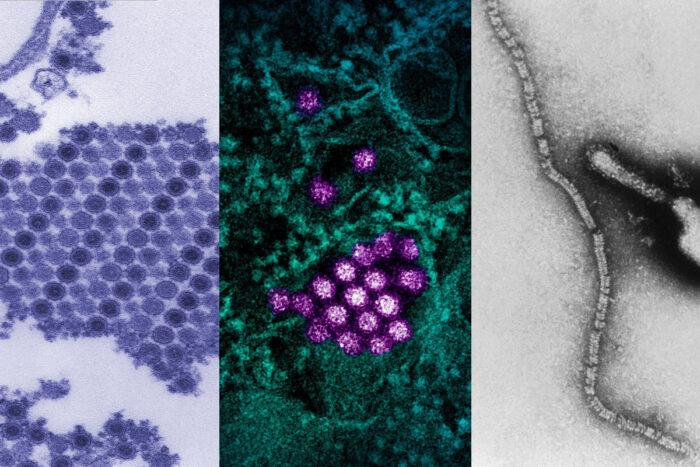 (l to r) CDC/Cynthia Goldsmith, James Comer, Barbara Johnson; CDC and NIAID; CDC/Erskine Palmer
(l to r) CDC/Cynthia Goldsmith, James Comer, Barbara Johnson; CDC and NIAID; CDC/Erskine PalmerWashU Medicine scientists lead two large, multicenter programs to develop vaccines and antibody-based therapies for understudied viruses with pandemic potential, including the three shown above: (left to right) chikungunya, dengue and parainfluenza viruses. The programs are supported by two grants from the National Institute for Allergy and Infectious Diseases (NIAID) totaling more than $30 million a year for three years.
Scientists at Washington University School of Medicine in St. Louis are laying the groundwork to rapidly respond to potential future pandemics caused by viruses from five understudied families. The effort, the aim of which is to develop strategies and tools to produce vaccines and antibody-based therapies in advance of future pandemic threats, is supported by two major grants from the National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health (NIH), which together will add up to more than $90 million in funding over the next three years.
One grant, totaling about $15.6 million per year for three years, is focused on the alphavirus and flavivirus families. These mosquito- and tick-borne viruses cause arthritis, brain infections and congenital disease, and the best-known members include dengue, Zika, West Nile and chikungunya viruses. The other grant, for $14.7 million per year for three years, takes aim at virus families that include respiratory pathogens such as mumps virus, as well as insect-borne viruses that cause high fevers such as Oropouche and Rift Valley fever viruses. Both grants are part of NIAID’s newly established Research and Development of Vaccines and Monoclonal Antibodies for Pandemic Preparedness (ReVAMPP) Network, and WashU Medicine researchers are leading two components of the network.
“If the COVID-19 pandemic taught us anything, it’s that being prepared saves lives,” said Michael S. Diamond, MD, PhD, the Herbert S. Gasser Professor of Medicine at WashU Medicine and the director of the ReVAMPP flavivirus and alphavirus program led by WashU Medicine. Diamond is also a professor of molecular microbiology and of pathology & immunology at WashU Medicine. “We had some preparation for the COVID-19 pandemic because of previous research on the related SARS and MERS viruses. But there are other viruses with potential to cause pandemics for which we are even less prepared. We don’t have specific therapies for any of the flaviviruses or alphaviruses, and we don’t know how to quickly make safe and effective vaccines for them, either.”
The research programs focus on one or two prototype viruses from each family, using them to develop and evaluate vaccine platforms and antibody-based treatment approaches that can be rapidly adapted to generate safe and effective vaccines and drugs for other members of the families in case of an emerging pandemic.
Some of the research at WashU Medicine will take place in specially designed laboratories known as biosafety level-3 (BSL-3) labs. Such labs provide a safe, secure environment for conducting research on highly infectious viruses and play a pivotal role in advancing understanding of infectious diseases.
“There’s no way to predict when and where the next pandemic virus will emerge, so we need to be prepared for all possibilities,” said Sean Whelan, PhD, the Marvin A. Brennecke Distinguished Professor and head of the Department of Molecular Microbiology at WashU Medicine. Whelan is the director of the ReVAMPP paramyxovirus, peribunyavirus and phlebovirus program led by WashU Medicine. “We are identifying the principles that determine a strong immune response for these virus families so we can apply those principles to rapidly design and produce protective vaccines as needed.”
 Related: Scientists aim to develop vaccine against all deadly coronaviruses
Related: Scientists aim to develop vaccine against all deadly coronaviruses
$8 million NIH grant supports effort to avert next pandemic
Viruses with pandemic potential
Flaviviruses and alphaviruses are spread by mosquitoes and ticks. Although most such viruses are uncommon, collectively they are responsible for tens of thousands of deaths annually, and they are spreading. Climate change and increased international travel make it easier for the insects and other small animals that carry these viruses to thrive in new parts of the world.
The Flavivirus and Alphavirus ReVAMPP (FLARE; grant number 1U19AI181960-01) program will develop prevention platforms for five prototype viruses representing the major subgroups of the flavivirus and alphavirus families. The team is led by Diamond with co-director Richard Kuhn, PhD, the Trent and Judith Anderson Distinguished Professor of Science at Purdue University and Krenicki Family Director of the Purdue Institute of Inflammation, Immunology and Infectious Disease, and collaborators at another 16 institutions nationwide. The prototype viruses are:
- West Nile virus, a mosquito-borne flavivirus that causes brain infections.
- Tick-borne encephalitis virus, a flavivirus that causes brain infections.
- Dengue virus, a mosquito-borne flavivirus that causes fever, headache, joint and muscle pain, and can progress to a severe shock syndrome. The most widespread virus in either family by far, dengue has four subtypes that create unique challenges for vaccine design.
- Chikungunya virus, a mosquito-borne alphavirus that causes debilitating acute and chronic arthritis.
- Venezuelan equine encephalitis virus, a mosquito-borne alphavirus that causes brain infections.
The other program is called Vaccines and Therapeutic Antibodies to Respiro, Rubula, Peribunya and Phenuiviridae (R2P2)-ReVAMPP (grant number 1U19AI181984-01). Respiroviruses and rubulaviruses are groups within the paramyxovirus family, and they cause common respiratory infections that can turn serious in vulnerable populations. Peribunyaviruses and phenuiviruses are two related families of bunyaviruses that are spread by insects or exposure to blood and cause uncommon but severe disease involving high fevers.
The R2P2 program is led by Whelan with co-directors Anne Moscona, MD, a professor of pediatrics at Columbia University Irving Medical Center, and Rino Rappuoli, PhD, the scientific director of the Fondazione Biotecnopolo di Siena in Italy, and collaborators at another 10 institutions across the U.S., Italy, Brazil and Germany. The team will be studying:
- Parainfluenza virus 3, a member of the respirovirus genus of the paramyxovirus family. Parainfluenza viruses are common causes of colds in healthy adults, but they can cause serious illness and death in infants, young children, older adults and people with compromised immune systems.
- Mumps virus, a member of the rubulavirus genus of the paramyxovirus family.
- Oropouche virus, a mosquito- and midge-borne peribunyavirus that causes fever, headache and body aches.
- La Crosse virus, a mosquito-borne peribunyavirus that causes brain infections, particularly in children.
- Rift Valley fever virus, a blood-borne and insect-borne phlebovirus that causes fever, headaches and bleeding in infected people. The virus also causes significant economic damage because it infects livestock, causing serious illness, pregnancy loss and death.
- Toscana virus, an insect-borne phlebovirus that causes high fever and brain and spinal cord infections.
Drafting solutions for rapid deployment
The FLARE and R2P2 teams aim to use the prototype viruses to develop and evaluate vaccine platforms that can be rapidly adapted to generate safe and effective vaccines for other viruses of these types.
In addition, the teams are working on optimizing antibody-based treatments. These drugs, commonly used to treat cancer and infections, are a crucial part of the pandemic response toolkit, because they can be developed much more quickly than other kinds of drugs for infectious diseases. The challenge is that viruses can develop resistance that undermines their utility, which is why all of the antibody-based therapies that were initially approved for COVID-19 became less useful as the virus evolved and were eventually withdrawn. The collaborative teams are investigating the scientific principles underlying human antibodies and their interactions with viruses with a goal of understanding how to quickly develop antibody-based drugs that will maintain their potency.






