$46 million supports research likely to result in new therapies, improve health care
NIH grant nurtures translational research
 Robert Boston
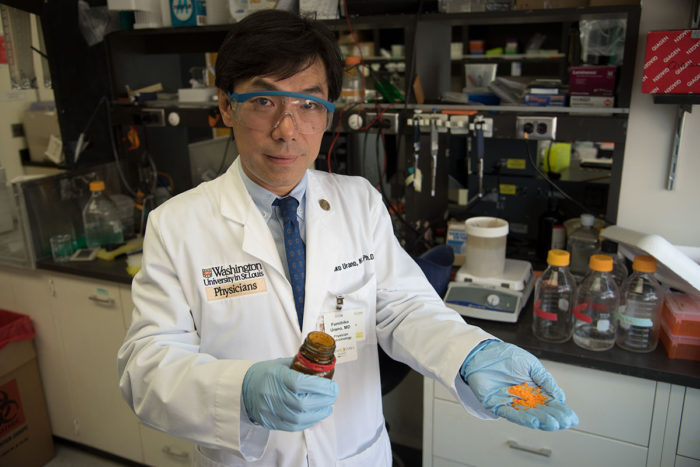
Robert BostonWashington University Professor Fumihiko Urano, MD, PhD, holds dantrolene, an FDA-approved muscle relaxant that his research has shown may treat Wolfram syndrome, a rare but devastating condition. The university's Institute of Clinical and Translational Sciences (ICTS), which supports research that is likely to result in new therapies for patients, helped Urano's team understand the disease in the lab and then create a translational pipeline to investigate the drug in patients with Wolfram syndrome.
Washington University School of Medicine in St. Louis has received a $46 million grant from the National Institutes of Health (NIH) to support research aimed at translating scientific and clinical discoveries into new diagnostics and therapeutics, and to more rapidly apply research findings to improve health.
The grant, from the National Center for Advancing Translational Sciences (NCATS), supports the School of Medicine’s Institute of Clinical and Translational Sciences (ICTS), one of 57 such centers in the United States.
Washington University’s ICTS works to advance clinical and translational sciences across the university and throughout the region. Rather than focus on a single disease or specialty, the resources and facilities supported by ICTS funds are intended to speed the adoption of research findings in disease prevention, diagnosis and treatment across the spectrum of health care.
“The School of Medicine sits at the epicenter of efforts to translate scientific discoveries into new therapeutics and better care for patients,” said David H. Perlmutter, MD, executive vice chancellor for medical affairs and dean of the School of Medicine. “Academic medical centers are uniquely positioned to coordinate all the complex machinery linking basic research at the lab bench to doctors eventually being able to prescribe resulting therapies to their patients. The mission of the ICTS is to facilitate this process, providing funds and resources at each step, so that the most up-to-date knowledge and latest discoveries move beyond the pages of scientific journals and into widespread practice.”
The Washington University ICTS is a regional consortium that includes important partnerships with BJC HealthCare, Saint Louis University, the St. Louis College of Pharmacy and the University of Missouri-Columbia.
Over the past decade, ICTS funds have supported many research efforts that have resulted in major steps forward in understanding and treating disease, including the development and testing of new diagnostic methods, new drugs and other therapies. Washington University’s ICTS has actively promoted the career development of students and junior faculty, many of whom are emerging as leaders in their fields.
In light of these successes, Bradley A. Evanoff, MD, director of the ICTS, highlighted the importance of the institute’s work focused on communicating the latest, best practices in medicine and ensuring that doctors across the country are implementing them.
“To improve health on a larger scale, the ICTS builds on Washington University’s many strengths,” Evanoff said. “We conduct research that advances the pace of discovery, and disseminates and implements research results to improve personal, community and population health. Scientists working on early-stage discovery are increasingly collaborating in teams with clinicians and other stakeholders to conduct research that will more directly lead to improvements in health. Close engagement between researchers and health-care providers allows the best methods for prevention, diagnosis and treatment to be more rapidly available to patients in a variety of settings.”
Victoria J. Fraser, MD, the Adolphus Busch Professor and head of the Department of Medicine, said another vital function of the ICTS is to train new clinical investigators and scientists who can bridge the gap between research and patient care.
“The intense training of new clinical investigators is a crown jewel of the program,” Fraser said. “Continuously supplying the long-term pipeline that creates extremely well-prepared scientists and clinical researchers is critical if we are to continue to be successful in turning knowledge into practice.”
Two investigators who came through rigorous ICTS training programs and are now standouts in their fields are Stephanie A. Fritz, MD, an associate professor of pediatrics, and Rupa Patel, MD, an assistant professor of medicine. Fritz’s work studying methicillin-resistant Staphylococcus aureus (MRSA) infections acquired in the community, rather than in hospital settings, has changed policy guidelines for helping families reduce recurrent MRSA infections. And Patel’s work has been instrumental in expanding the use of Pre-Exposure Prophylaxis (PrEP), a medication that lowers the chance of infection with human immunodeficiency virus (HIV) among people at high risk of HIV infection. Patel is the program director for PrEP at the Washington University Infectious Disease Clinic and a member of the World Health Organization’s Technical Advisory Group for PrEP.
Another example of major progress made expeditiously with ICTS support involves Zika virus, particularly understanding it as it emerged and was linked to newborn microcephaly, a birth defect in which the brain does not develop properly. ICTS support helped virologist Michael S. Diamond, MD, PhD, the Herbert S. Gasser Professor of Medicine, team up with fertility expert Kelle H. Moley, MD, the James P. Crane Professor and vice chair of obstetrics and gynecology, to discover that Zika infection in males results in significant damage to the testis and resulting reproductive dysfunction. Diamond, in collaboration with Indira Mysorekar, PhD, an associate professor of obstetrics and gynecology, was among the first to model Zika infection in pregnant mice, determine how the virus is transmitted across the placenta and begin to find ways to block it. This research has led to the development of investigational antibodies and vaccines that may target or protect against Zika virus.
 Huy Mach
Huy MachAnother example of the breadth of ICTS’ success is the recent development of a translational pipeline for the treatment of Wolfram syndrome.
The syndrome is a rare cause of diabetes and visual impairment in children that also affects many other organs, including the brain. With ICTS support, Washington University researchers led by Fumihiko Urano, MD, PhD, created a clinical and translational research program to study the disease, which led to fundamental laboratory studies that uncovered the molecular genetic defect, and ultimately to the identification of a therapeutic target that is now being tested in patients. According to Urano, the Samuel E. Schechter Professor of Medicine, national resources offered through the NCATS Rare Disease Program combined with patient organizations and local ICTS support have directly supported the first clinical trial of a repurposed drug for the treatment of Wolfram syndrome.
A new grant led by the Urano team and funded by NIH/NCATS will combine elements of collaborative preclinical science with the national drug development team at NCATS, along with later clinical trial staging. The novel bench testing approach paired with therapeutic strategies will deliver personalized medicine for patients with Wolfram syndrome and other forms of juvenile diabetes.
Evanoff is enthusiastic that the next phase of the ICTS funded by the $46 million award will support the career development of a new generation of translational scientists and ensure the success of promising translational research at Washington University and across the region.






