Emergency Operations Center responds to COVID-19
Medical school, Barnes-Jewish Hospital face challenge together
 Matt Miller
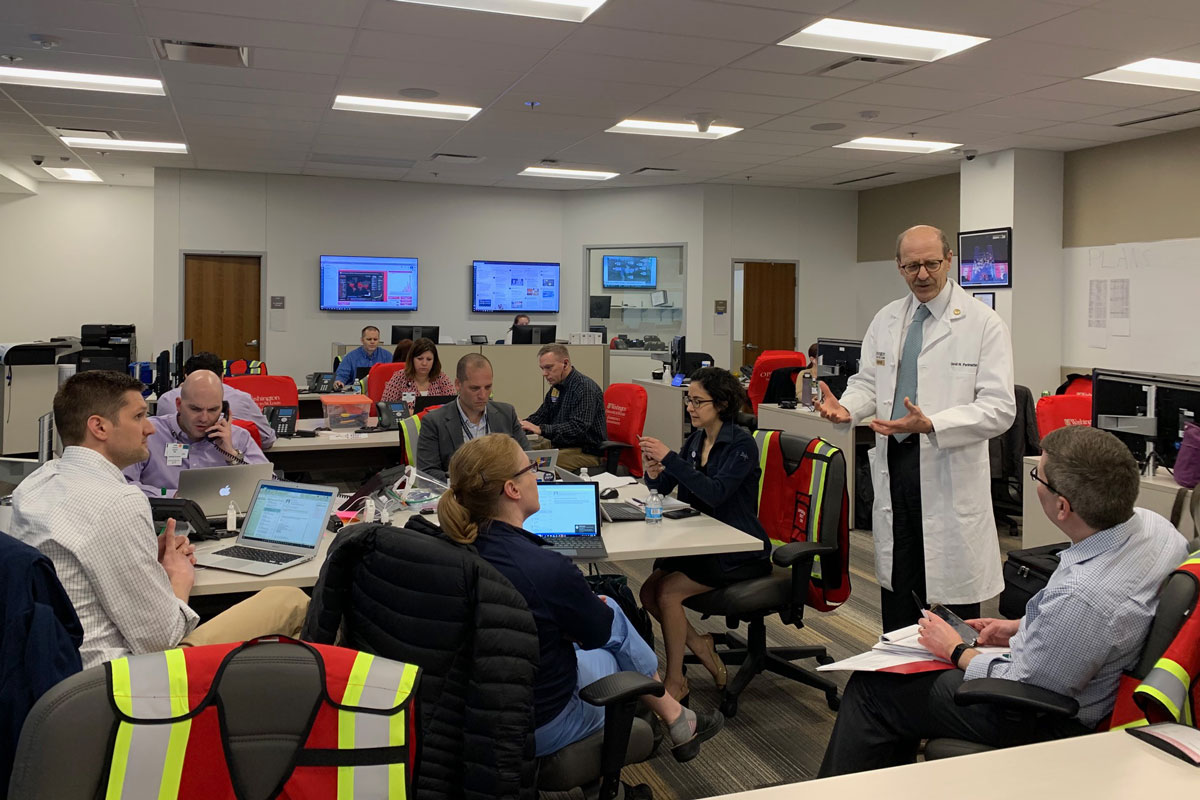
Matt MillerIn response to the coronavirus pandemic, public safety employees from Barnes-Jewish Hospital and Washington University School of Medicine work together in early April in the Emergency Operations Center (EOC) in the Mid Campus Center. Shown are David Warren, MD, a professor of medicine in infectious diseases, and Patrick Aguilar, MD, an assistant professor of medicine in pulmonary and critical care medicine. Both are part of the EOC's medical branch.
In the three years since it opened, the Emergency Operations Center (EOC) on the Washington University Medical Campus has successfully weathered smaller-scale crises in the form of water main breaks, power outages and ice storms.
But the center’s major test arrived in March, when scientists classified the spread of the novel coronavirus as a pandemic and COVID-19 cases began appearing in all 50 states.
“The coronavirus is our first large-scale crisis,” said Ty Davisson, director of emergency management at Washington University in St. Louis. “It’s all hands on deck.”
The Emergency Operations Center serves as the Medical Campus’ central command for responding to the pandemic. Housed on the first floor of the Mid Campus Center, the EOC unites representatives from the School of Medicine and Barnes-Jewish Hospital (BJH) in one location. There, they work behind the scenes to provide rapid, coordinated responses to emergencies such as tornadoes, earthquakes, civil unrest and the ongoing coronavirus outbreak.
The EOC’s coordination extends beyond the medical school and BJH. The center integrates information from crisis management teams on the Danforth Campus and at St. Louis Children’s Hospital and throughout BJC HealthCare.
At any given time during the COVID-19 crisis, the EOC hosts representatives in person and via Zoom, including senior leadership, physicians and other clinical staff, as well as employees with expertise in planning and operations, logistics and supply chains, technology and information systems, human resources, environmental health and safety and communications. Social distancing is required. Hand sanitizer and alcohol wipes are used regularly to disinfect all computer and physical surfaces.
“The purpose is to have all the key decision-makers and players present in one place, at a safe distance, so we have a common picture of the rapidly evolving situation,” Davisson said. “This allows us to exchange critical information and make decisions quickly while all being on the same page.”
In response to a growing number of COVID-19 patients in the St. Louis region, the EOC has been activated with staff monitoring coronavirus developments globally, nationally, regionally, as well as on the Medical Campus. Staff in the EOC also plan for the care of patients with COVID-19, working to ensure adequate numbers of hospital beds and ventilators, and the safety of front-line health-care professionals, including whether they have enough personal protective equipment such as face shields, masks, gloves and gowns. Others coordinate staffing levels among health-care workers and other essential staff, such as housekeeping. As the number of COVID-19 cases increased in the St. Louis region, the EOC team worked to set up employee and visitor screening stations to check for symptoms, and an employee testing area for those who develop symptoms at work or who are exposed to the virus.
“One of the challenges in establishing the employee screening program and setting up a COVID testing area for employees was ensuring that these initiatives not only were workable for the School of Medicine but for all employees at the hospitals and across BJC,” said Sherry Banez-Muth, clinical operations director for the Faculty Practice Plan. “We worked in close collaboration in ways we haven’t needed to before.”
Employee mental health has been another top priority for the EOC. Staff in Human Resources worked closely with the Department of Psychiatry to establish resources and a hotline to ensure that employees on the Medical Campus have support to cope with stress, anxiety and depression during uncertain times.
“The EOC is an immense operation, with critical decisions being made every day to ensure that patients get the best medical care possible and that health-care workers and other staff have what they need to get through this challenging time,” said School of Medicine COVID-19 lead Paul J. Scheel, MD, associate vice chancellor for clinical affairs and CEO of Washington University Physicians. He works closely with Bob Cannon, Barnes-Jewish Hospital president and BJC HealthCare group president, who is leading the COVID-19 BJC Incident Command Center operations, and John Lynch, MD, who is serving as the BJH executive leader in the Washington University Medical Campus EOC.
The EOC’s high-tech workspace can accommodate up to 75 people, with designated work stations that encourage open lines of communication — critical in fast-moving situations. But during the pandemic, there are typically no more than 20 people in the room so on-site staff can maintain social distancing. A 50-foot-by-5½-foot video wall displays the latest statistics and graphs on large screens, easily visible to anyone working in the EOC. It includes key data such as the number of hospitalized patients at BJH and each of the BJC HealthCare system hospitals, the number of hospital and ICU beds available, the number of COVID-19 cases in Missouri and the United States over time, as well as local and national news.
“The EOC and its staff have been incredible at overcoming the daily, sometimes hourly, challenges posed by the coronavirus outbreak,” added David H. Perlmutter, MD, executive vice chancellor for medical affairs, the George and Carol Bauer Dean of the School of Medicine, and the Spencer T. and Ann W. Olin Distinguished Professor. “We have had to work through changes in almost all of our operations, and the teamwork between WashU and BJH, SLCH and the rest of the BJC system has been magnificent.”
The collaboration has been key to the EOC’s success. “COVID-19 is the EOC’s first large-scale emergency, the first big test,” said John Lynch, MD, chief medical officer and chief operations officer at BJH. “It is challenging, to be sure, but the coordination and cooperation between the two institutions has been remarkable.”
Added Cannon: “The team has shown great skill in being able to adapt and respond to a constantly changing situation, 24 hours a day. It is difficult to imagine how we would be managing this pandemic without the resources and structure of the EOC.”
Although the EOC develops emergency preparedness plans and conducts training programs for a pandemic, the coronavirus surprised everyone. “Based on medical expertise and government reports, we thought that if a pandemic were to occur, it would involve a strain of the flu,” said Ryan Nicholls, the School of Medicine’s assistant director of emergency management. “The scenario involving COVID-19 has rapidly evolved, and we’re learning as we go.”
Unique coronavirus challenges include the highly contagious and life-threatening nature of the virus and the need for social distance to prevent its spread.
“We have never worked in a crisis in which the first responders are so susceptible to becoming sick,” said Nicholls, who, along with Davisson, worked in Joplin, Mo., after a devastating tornado there in 2011. “Social distancing has added a whole new dynamic. At times, we have to communicate in person and work together because it cannot be avoided when dealing with a crisis. But we practice social distancing as much as we can by standing at least 6 feet apart and using Zoom and other technologies.
“The professionalism and overall compassion of people working in the EOC has helped us manage a fast-moving health crisis as seamlessly as possible,” he added.
 Joni Westerhouse
Joni Westerhouse





